Understanding Insomnia and Its Complex Relationship with Escitalopram
Everyone and their grandmother probably know what insomnia is, right? But let's gently pull apart the layers for a fuller understanding. In the simplest of terms, insomnia is a cruel joke played by Morpheus, the Greek god of dreams, where despite your best efforts, you just can't drift off into the peaceful abyss of sleep. Clinically speaking, it is a sleep disorder that makes it difficult for people to fall asleep, stay asleep, or both. And boy, do I know insomnia. I've had nights where my Beagle, Dexter, could be heard snoring comfortably and my Maine Coon, Willow, would be lost in a world of cat dreams. Me? I'd be wide awake, counting the spectral sheep that never quite jumped over the moon.
Now slip in Escitalopram into this mix. It's an antidepressant that belongs to a group of drugs known as selective serotonin reuptake inhibitors (SSRIs). It's commonly prescribed to treat depression and generalized anxiety disorder, but unfortunately, its interaction with insomnia can be a bit taxing. But don't worry. This isn't another Greek tragedy, and there are ways to cope!
Before You Take That Pill: Consider Your Lifestyle
Before we dive into the tips on coping with insomnia when taking Escitalopram, let's shift our gaze for a moment. Lets' take a look at our lifestyles. Lifestyle habits have a massive impact on our sleep cycles, more than you might believe. And admit it or not, we're all a bit guilty of pushing our bodies a little too hard and not giving them the rest they need. So, it's not just Dexter and Willow who deserve their beauty sleep, we need it too!
Remember those late-night binge-watching sessions, the bottomless cups of caffeine, those erratic meal times, and the chronic blue light exposure from gadgets? They all could be sabotaging your sleep while Escitalopram takes up all the blame. The first step in dealing with insomnia during Escitalopram therapy is making sure you correct any unhealthy lifestyle habits that may stand in your way. Trust me, with a few tweaks here and there, you might find yourself channeling your inner sleepy Maine Coon in no time!
Cope and Conquer: Lifestyle Changes to Improve Sleep
So you've taken stock of your lifestyle, and ready for those changes, huh? Great decision! Let's start with some practical and easy-to-adapt strategies that anyone can implement. First on the list is good sleep hygiene. Yes, it's a thing! Just like you wouldn't skip brushing your teeth (at least I hope not), practicing healthy sleeping habits must be a non-negotiable. This means a consistent sleep schedule, a dark, quiet, and cool bedroom, and a comfortable bed (one that's not already dominated by Dexter and Willow).
If you're a caffeine fiend, I hate to be the bearer of bad news, but it's time to cut back or at least monitor your intake. During my personal battle with insomnia, I went from a casual, two cups of coffee a day drinker to completely eliminating it. And honestly, the results were simply amazing! And those late-night tech sessions with your devices? It might be time to institute a gadget curfew to allow your mind to wind down for an effective transition into sleep.
The Power of Exercise and Right Nutrition
Did you think that only your high school gym teacher would harp on the benefits of exercise? Wrong! Exercise has this magical knack for tiring us out in the best of ways, making it easier for us to fall asleep. Now I am not suggesting you train for a triathlon right away, but introducing moderate exercise into your daily routine could work wonders. Speaking from personal experience, when I involved a half-hour walk in my evenings, my sleep improved markedly.
Moving on to our plates, the food we consume also plays a critical role in our sleep. Avoid heavy, spicy, or high-sugar foods close to bedtime. Instead, opt for a small, balanced snack if hunger pangs come knocking. Interestingly, certain foods can promote sleep, like almonds, walnuts, chamomile tea, and kiwi. So, next time when insomnia is playing hardball, try munching on these sleep-inducing goodies.
Mental Health over Matter: Therapies and Relaxation Techniques
When taking Escitalopram, it's crucial to include mental relaxation techniques in your insomnia-fighting toolbox. Stress and anxiety can be key factors causing insomnia. And techniques such as mindfulness, meditation, and yoga can greatly help in reducing them. Therapies such as Cognitive Behavioral therapy for Insomnia (CBT-I) can also play a pivotal role in managing sleep disturbances. This approach helps you challenge and change thought patterns leading to insomnia and eventually develops healthy sleeping habits.
While I am not a yoga fanatic, I have found incorporating a short session of calming yoga poses before bed surprisingly relaxing. And don't even get me started on the magical charm of a relaxing hot bath for lulling you into sleep. Pro tip: A dash of lavender oil in your bath can take the relaxation factor up several notches.
Prescriptive Measures: A Guiding Light from Physicians
If your sleep issues persist despite tweaking your lifestyle habits, incorporating exercise, good nutrition habits, and relaxation techniques, then it's time to consult your doctor. After all, it's their job to guide us through the labyrinth of medical conditions and medications. Keep in mind that Escitalopram takes about 4-6 weeks to work fully, and initial side effects like sleep disturbances might settle down after this period. Stay in close contact with your doctor, and never hesitate to discuss any persisting sleep problems. A possible outcome might be a decrease in dose, a shift in the medication timing, or maybe a switch to another drug.
Before you freak out over the 'switching the drug' part, know that there are dozens of other options available. Every individual is unique and responds differently to medications, so finding the right drug might involve a little bit of trial and error. But remember, under the vigilant guidance of your doctor, you'll surely be okay. And you are not alone in this. Many have successfully braved this journey before, and so can you.
When All Else Fails: Considering Sleep Aids
Lastly, if insomnia stands stubborn and lifestyle changes, relaxation techniques, or an adjustment in medications doesn't help, then sleep aids might be discussed with your doctor. However, I must reinforce here: Always use sleep aids under the supervision and prescription of a healthcare provider. Non-prescription or 'over-the-counter' sleep aids can provide temporary relief, but they are not intended for long-term use and may even contribute to the problem if used incorrectly.
In my personal journey, there was a time when, despite trying everything, sleep was elusive. I ended up resorting to sleep aids, but only for a brief period, and under close medical supervision. The experience wasn't a joyride, but it was comforting to know that I had someone to guide me through it. Throughout this part, commit to staying in touch with your healthcare provider and make well-informed decisions.
Final Nightcap: Sleep Troubles & Escitalopram – The Curtain Close
Insomnia, at its core, is an unwelcome guest in our lives, and when it decides to partner with Escitalopram, things might seem a bit daunting. But remember: every cloud has a silver lining. You are armed now with numerous strategies to cope with these night-time foes. Tailored lifestyle changes, proper nutrition, physical exercise, focused mental health practices, regular check-ups with a physician, and sleep aids as last-case scenarios can combine to ease your sleepless nights immensely.
In closing, I'd like to say that coping with insomnia while on Escitalopram is unequivocally possible. It’s about acknowledging and dealing with factors that might be contributing to your insomnia. It's about communicating with your healthcare provider to ensure you're on the right track. It's about realizing you’re not alone, and there's plenty of help and support available. And it's about remembering that, just like my quirky companions Dexter and Willow, you too have every right to some darn good sleep. So don't lose heart, sweet dreams are just around the corner!









Honestly, if you're not willing to ditch that midnight caffeine binge, you're just asking for trouble.
Sleep is a right, not a luxury, and you owe it to yourself to respect it.
I totally get how hard it can be to change those late-night habits, and I'm here to say you're not alone in this.
We can all benefit from a little cultural exchange of sleep tips, like swapping out that 4pm coffee for a soothing herbal tea.
Remember, small steps like setting a consistent bedtime can cascade into big improvements.
And if you ever need a buddy to share your progress, just shout – we love supporting each other!
When addressing SSRI-induced insomnia, one must first consider the pharmacokinetic profile of escitalopram, specifically its half-life and receptor affinity.
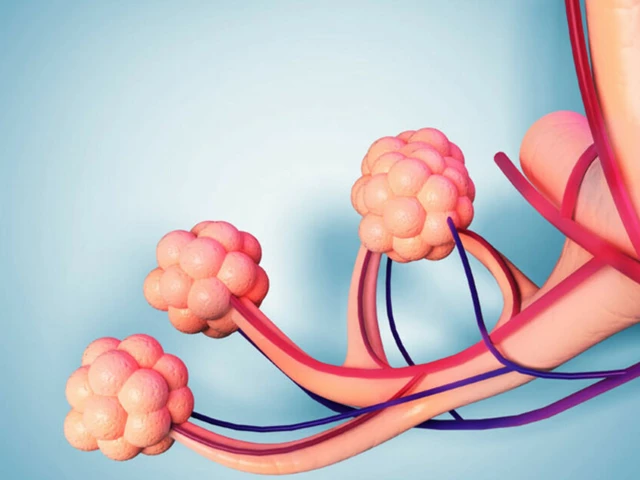
The drug exhibits a relatively long elimination half-life, which can lead to residual serotonergic activity during nocturnal periods.
Consequently, the hypothalamic-pituitary-adrenal axis may experience dysregulation, manifesting as heightened arousal states.
From a neurochemical standpoint, the upregulation of 5-HT2A receptors can attenuate the homeostatic drive for sleep.
Mitigating these effects often requires a multimodal approach that integrates both behavioral and pharmacological interventions.
Implementing cognitive-behavioral therapy for insomnia (CBT-I) is considered first-line due to its robust evidence base.
In addition, the timed administration of the medication-preferably in the morning-can reduce nocturnal serotonergic spillover.
Adjunctive agents such as melatonin receptor agonists may be employed to realign circadian rhythms, provided there are no contraindications.
Furthermore, exercise physiology suggests that moderate aerobic activity performed 3-4 hours prior to bedtime can enhance sleep efficiency by up to 15%.
Nutritionally, ingesting foods rich in tryptophan can serve as a precursor to melatonin synthesis, thereby supporting endogenous sleep pathways.
From a clinical monitoring perspective, one should utilize validated scales like the Insomnia Severity Index (ISI) to quantify therapeutic response.
If refractory insomnia persists beyond six weeks, a dosage adjustment or a switch to an alternative SSRI with a more favorable sleep profile, such as sertraline, may be warranted.
Always ensure that any pharmacologic augmentation, such as low-dose trazodone, is prescribed under strict supervision to avoid additive sedation.
Patient education remains paramount; individuals should be counseled on sleep hygiene, caffeine restriction, and screen time curtailment.
In summary, a systematic, evidence-based regimen-combined with patient adherence-can substantially ameliorate SSRI-related sleep disturbances 😊.
Your comprehensive overview highlights the importance of a structured, evidence‑based plan when tackling escitalopram‑related insomnia.
By prioritizing CBT‑I and considering medication timing, you address both behavioral and pharmacological dimensions.
Additionally, the recommendation to monitor progress with standardized tools such as the ISI ensures objective assessment.
The inclusion of lifestyle factors – exercise, nutrition, and screen hygiene – reinforces a holistic approach.
It is encouraging to see an emphasis on patient education, as informed individuals are more likely to adhere to interventions.
Overall, your strategy balances rigor with practicality, offering a clear roadmap for clinicians and patients alike.
Sure, the pharma giants want you sleepless so they can sell more pills!!!