Back pain that won’t quit. A dull ache that turns sharp when you stand up. Numbness creeping down your leg. If you’re over 50 and dealing with these symptoms, it might not just be "old age"-it could be spondylolisthesis. This isn’t a rare condition. About 6 in every 100 adults have at least one vertebra that’s slipped out of place, usually in the lower back. For many, it’s silent. But for others, it’s life-limiting. The good news? You don’t have to just live with it. Understanding what’s happening-and your real options-is the first step to feeling better.
What Exactly Is Spondylolisthesis?
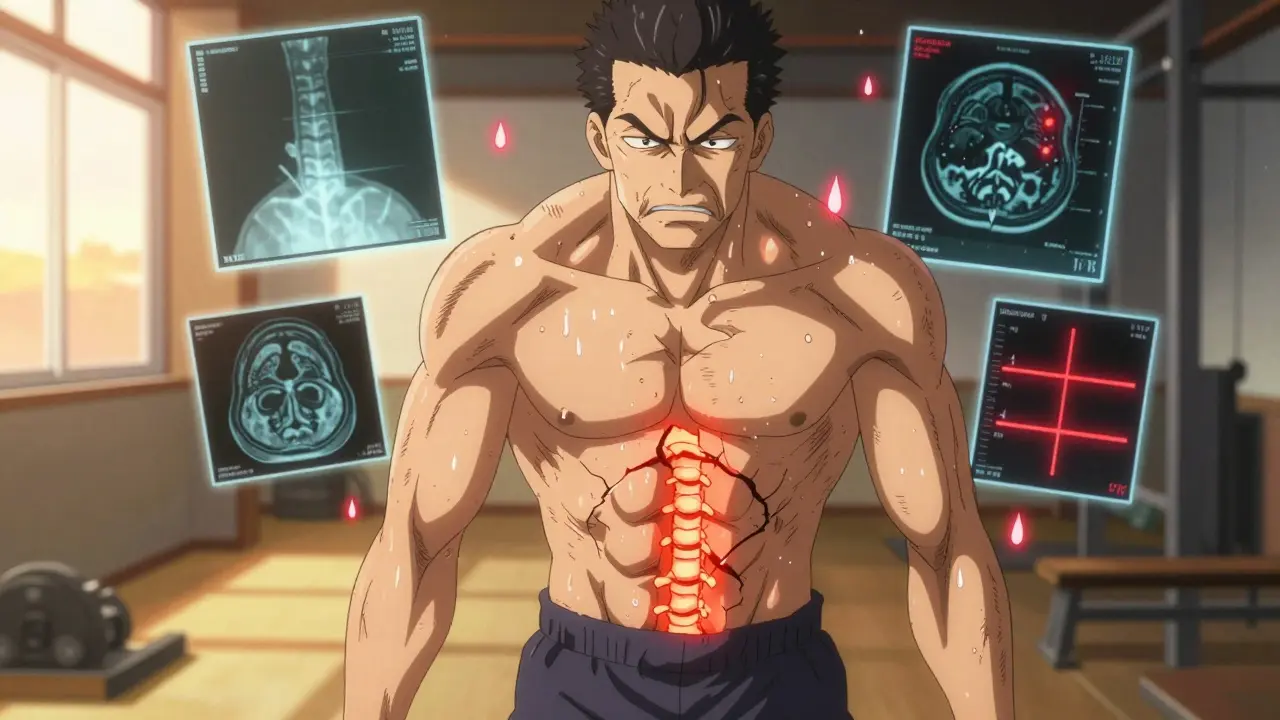
Spondylolisthesis means one of your spinal bones (a vertebra) has slid forward over the one below it. Think of it like a stack of blocks where one block has shifted a little. It’s most common between the fifth lumbar vertebra (L5) and the first sacral bone (S1). That’s the bottom of your lower back, right above your tailbone. The slip isn’t always dramatic-some are barely 10% out of place. Others can slide more than half the width of the bone. Doctors use the Meyerding scale to grade it from I (mild) to IV (severe).It’s not one condition-it’s five. The most common type in adults over 50 is degenerative. That’s from wear and tear. Arthritis breaks down the discs and joints that hold your spine together. As they give way, the vertebra slips. In younger people, especially athletes, it’s often isthmic. That’s a tiny stress fracture in the part of the bone that connects the joints. Gymnasts, football players, and weightlifters are at higher risk because their sport forces the spine into repeated backward bends. Less common are types caused by birth defects, tumors, or trauma.
Why Does It Hurt?
Not everyone with a slipped vertebra feels pain. In fact, about half of people with spondylolisthesis never know they have it. But when it does cause problems, the pain is usually deep in the lower back. It feels like a muscle strain, but it doesn’t go away with rest the way a pulled muscle would. Standing or walking makes it worse. Sitting or leaning forward often brings relief-that’s because those positions take pressure off the nerves.One of the most telling signs? Tight hamstrings. About 70% of people with symptomatic spondylolisthesis can’t touch their toes without discomfort. That’s not just tight muscles-it’s your body’s way of protecting the spine. Your hamstrings pull on the pelvis, and if they’re too tight, they change how your spine sits, adding strain.
If the slip is severe (Grade III or IV), you might start feeling tingling, numbness, or weakness in one or both legs. That’s nerve compression. The slipped bone is pressing on the spinal nerves that run down to your legs. In advanced cases, your posture can change. You might develop a swayback, then later, a rounded upper back (kyphosis) as your spine tries to compensate.
How Is It Diagnosed?
Your doctor won’t guess. They’ll start with a simple standing X-ray. That’s the gold standard. It shows exactly how far the bone has slipped. A CT scan gives a clearer picture of the bones-useful if there’s a fracture or if surgery is being considered. An MRI is the key to seeing soft tissue: which nerves are pinched, how much disc degeneration there is, and whether inflammation is present.Here’s something important: the degree of slip doesn’t always match how much pain you feel. A person with a Grade I slip might be in agony, while someone with a Grade IV might barely notice. That’s because pain comes from nerve pressure and inflammation-not just how far the bone has moved. Research shows disc degeneration, not the slip itself, correlates more strongly with symptoms. That’s why treatment focuses on what you’re feeling, not just what the X-ray shows.

Conservative Treatment: What Actually Works
Most people don’t need surgery. The first line of defense is conservative care-and it works for most. But it takes time and consistency.- Physical therapy is the cornerstone. A good program focuses on strengthening your core (abdominals and lower back muscles) and stretching your hamstrings. You’ll need 12 to 16 weeks of regular sessions to see real results. Only about two-thirds of people stick with it long enough.
- Activity modification means avoiding movements that make it worse. If you’re a runner, you might switch to swimming or cycling. If you lift weights, you’ll need to drop the heavy squats and deadlifts. Even simple things like sitting in a chair with good lumbar support help.
- NSAIDs like ibuprofen or naproxen can reduce inflammation and pain. But they’re not a long-term fix. They mask the problem, they don’t fix it.
- Epidural steroid injections can help if nerve pain is the main issue. They’re not a cure, but they can give you a window of relief-often 3 to 6 months-to get into therapy and build strength.
Doctors usually recommend trying these for at least 6 to 12 months before considering surgery. If your pain hasn’t improved, or if you’re losing strength in your legs, it’s time to talk about more serious options.
Spinal Fusion: The Main Surgical Option
When pain is constant, mobility is gone, and nerves are being squeezed, fusion becomes the most reliable solution. The goal isn’t just to stop the slip-it’s to stop the pain by fusing the unstable vertebrae together so they become one solid bone.There are three main ways to do it:
- Posterolateral fusion (55% of cases): Bone graft is placed along the back of the spine, and screws and rods are used to hold everything in place. It’s been the standard for decades. Success rates are 75-85% for mild slips, but drop to 60-70% for severe ones.
- Interbody fusion (35% of cases): This is the most effective approach today. The surgeon removes the damaged disc and inserts a spacer between the vertebrae. This restores disc height, opens up the space where nerves exit the spine, and gives the bone graft a better surface to grow on. Two common types are PLIF (from the back) and TLIF (a less invasive version). Success rates? 85-92% across all slip grades.
- Minimally invasive techniques (10% of cases): Smaller incisions, less muscle damage, faster recovery. These are growing in popularity, especially for younger, healthier patients.
Here’s the truth: if you have a severe slip (Grade III or IV), interbody fusion is your best bet. It’s more complex, but it gives you a much higher chance of lasting relief.

What You Need to Know Before Surgery
Fusion isn’t a quick fix. It’s a major procedure with a long road to recovery. Here’s what really matters before you sign off:- Stop smoking. Smokers are 3.2 times more likely to develop pseudoarthrosis-that’s when the bones don’t fuse properly. Quitting even 6 weeks before surgery improves your odds dramatically.
- Manage your weight. A BMI over 30 increases surgical complications by nearly 50%. Losing even 10 pounds can make a big difference in healing and reduce stress on the fusion site.
- Expect a long recovery. You’ll need 6 to 8 weeks of limited activity. Physical therapy starts around week 4 and lasts 3 to 6 months. Full healing? It can take 12 to 18 months. Your spine needs time to knit together.
Success rates are high-85-92% for interbody fusion-but they’re not perfect. About 12-15% of people with severe slips need a second surgery. Why? Adjacent segment disease. When one part of the spine is fused, the segments above and below it take on more stress. Over time, that can lead to degeneration there too. About 1 in 5 people develop this within 5 years.
Newer Options and What’s Coming
The field is evolving. In 2022, the FDA approved two new interbody devices designed specifically for spondylolisthesis. Early results show 89% fusion rates at 6 months-better than older models.Biologics are also being tested. Bone morphogenetic protein (BMP) and stem cell therapies are showing promise. A 2023 study found BMP-2 pushed fusion rates to 94% in high-risk patients, compared to 81% with traditional bone grafts.
But not everyone needs fusion. For mild slips, dynamic stabilization devices are being used. These are like braces for the spine-allowing some movement while reducing pain. Success rates are around 76% after 5 years. That’s lower than fusion, but it’s an option for people who want to avoid fusing their spine entirely.
The global spinal fusion market is growing fast-projected to hit $7.8 billion by 2027. That’s because more people are living longer, and degenerative spine issues are rising with age. But the real breakthrough isn’t in the hardware-it’s in better patient selection. A 2023 study identified 11 clinical and imaging signs that predict surgical success with 83% accuracy. That means fewer people get unnecessary surgery.
When to Act-and When to Wait
If your back pain has lasted more than 3 to 4 weeks, or if you’re having trouble walking, or numbness is creeping into your legs, see a doctor. Don’t wait until you can’t stand up straight.But don’t rush into surgery either. Give conservative care a real shot. Stick with physical therapy. Lose the extra weight. Quit smoking. These aren’t just "nice to haves"-they’re the difference between success and failure.
Spondylolisthesis isn’t a death sentence. It’s not even a life sentence. With the right approach, most people get back to living without constant pain. The key is knowing your options-and choosing the one that fits your body, your lifestyle, and your goals-not just what looks easiest on paper.
Can spondylolisthesis heal without surgery?
Yes, in most cases. About 80% of people with spondylolisthesis manage their symptoms successfully with physical therapy, activity changes, and pain management. Surgery is only considered when conservative treatments fail after 6 to 12 months and pain or nerve symptoms severely limit daily life.
Is walking bad for spondylolisthesis?
It depends. Walking can worsen pain if your spine is unstable and nerves are compressed. But complete inactivity makes things worse. The goal is modified walking-shorter distances, using a cane or walker for support, avoiding hills or uneven surfaces. Many patients find that walking in a slightly forward-leaning posture (like pushing a shopping cart) reduces pressure on the spine and eases discomfort.
What’s the difference between spondylolysis and spondylolisthesis?
Spondylolysis is a stress fracture in the pars interarticularis-a small bone segment that connects the joints in the spine. Spondylolisthesis is when that fracture causes the vertebra to slip forward. So, spondylolysis can lead to spondylolisthesis, but not everyone with a fracture will have a slip. Think of spondylolysis as the crack, and spondylolisthesis as the resulting movement.
How long does it take to recover from spinal fusion?
Recovery happens in stages. You’ll be restricted from heavy lifting and twisting for 6 to 8 weeks. Physical therapy usually starts around week 4 and lasts 3 to 6 months. Most people return to light work in 3 to 4 months, but full bone healing takes 12 to 18 months. Patience is key-rushing back too soon increases the risk of fusion failure.
Are there alternatives to spinal fusion?
For mild to moderate slips, dynamic stabilization devices are an option. These implants allow limited motion while reducing pain and pressure on nerves. They’re not for everyone-especially not for severe slips or older patients with significant bone loss. Long-term data is still limited, but early results show about 76% success at 5 years, compared to 88% for fusion. Research is ongoing.
Can spondylolisthesis get worse over time?
Yes, especially if you’re active in high-risk sports or have degenerative changes. In older adults, the slip can progress slowly as arthritis worsens. In younger people with isthmic spondylolisthesis, the slip may stabilize after growth stops. But without proper management-like core strengthening and avoiding hyperextension-it can worsen. Regular monitoring with X-rays is recommended if you’re at risk.




Bro, I had a Grade II slip and did PT for 6 months. Zero results. Then I got the TLIF. Now I’m hiking in Banff like nothing happened. Don’t waste your life on stretches if your spine is basically a Jenga tower. 🏔️💪
I love how this post breaks it down without making you feel like a broken machine. I’m 58 and started PT last year-my hamstrings are finally not screaming every morning. It’s slow, but I’m actually walking to the store again. 🌱
I’ve got degenerative spondylolisthesis and I’m 62. Didn’t do anything for 3 years. Then I got a cane and started swimming. Not magic. Just less pain. I’m not cured but I’m not crying in the shower anymore either
I used to think my back pain was just "getting old" until I found out my L5 had slid like a rogue skateboard. PT saved me. Not because it was easy-but because it made me feel like I still had control. Also, stretching your hamstrings feels like a betrayal at first… but then it’s like your body finally hugs you back 🤗
Oh wow. So you’re telling me I don’t need to drop $50k on fusion just because I can’t touch my toes? My yoga instructor said I was "energy blocked." I’m just glad I didn’t buy that.
This is the most accurate thing I’ve read in years. People think pain = damage. No. Pain = your nervous system screaming because you ignored it for 10 years. Stop Googling "miracle cures" and start doing the boring stuff. Core work. Hamstring stretches. Stop sitting like a potato. You’re not special. Your spine doesn’t care how cool your posture is on TikTok.
I want to emphasize-STOP SMOKING. I’m a 60-year-old former smoker who had a TLIF. My surgeon said my bone density was like wet cardboard. I quit cold turkey 8 weeks before surgery. Two years later? Fusion is solid. No pseudoarthrosis. No second surgery. Don’t be the guy who ignores the #1 modifiable risk factor. Your spine will thank you. Seriously.
They say fusion is the answer. But what if the real problem is we’re not meant to live past 70? We force our bodies to survive decades they weren’t designed for. Maybe the spine slips because it’s tired of holding us up through Zoom calls and bad coffee. Maybe it’s not a disease… it’s a protest.
Canada and India posting about back pain? I’m shocked. In the US we fix this with surgery, protein shakes, and a damn American flag on the hospital bed. No one here waits 12 months for PT. We go in, fuse it, and get back to work. If you can’t afford that, maybe you shouldn’t have moved here.
Fusion? That’s just the spine’s version of giving up. Why not just glue your vertebrae together? Oh wait-you’re doing that. You’re not healing. You’re turning yourself into a human statue. The real question: why are we so afraid of movement? Maybe the spine doesn’t need fusing… maybe it needs freedom.
I did PT for 8 months and now I can play with my grandkids without wincing. It’s not glamorous. But it’s real. You got this! 💪❤️
fusion isn’t the end it’s just the next step