Blood clots: how to spot them, prevent them, and act fast
A clot that starts in a leg can become a life-threatening problem if it travels to the lungs. Knowing the common signs, the biggest risks, and simple steps to lower your chance can save you time, worry, and maybe your life.
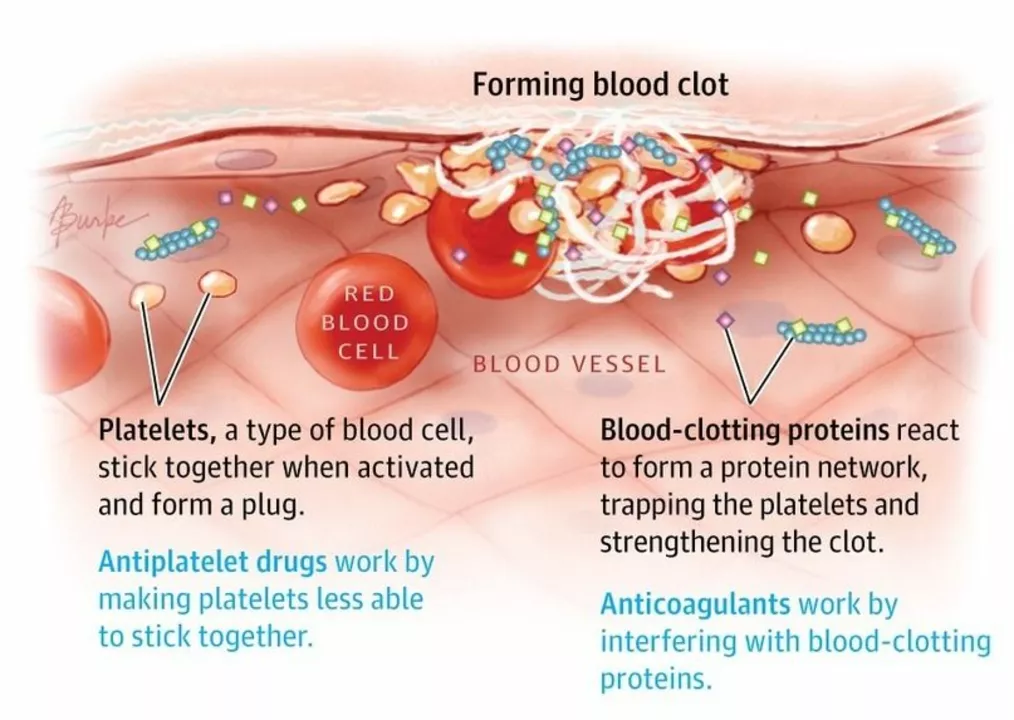
Blood clots form when blood thickens and sticks together. That’s normal after an injury, but clots that form inside veins or arteries without a clear reason can block blood flow. Two types matter most: deep vein thrombosis (DVT), usually in the legs, and pulmonary embolism (PE), when a clot reaches the lungs.
Signs and when to worry
DVT often shows as one leg that’s swollen, warm, painful, or red. It can feel like a cramp that doesn’t go away. PE causes sudden shortness of breath, sharp chest pain (worse with a breath), fast heartbeat, fainting, or coughing up blood. If you see any of those PE signs, get emergency care right away.
Clots can also affect the brain (stroke) or heart (heart attack). Stroke signs include sudden face droop, arm weakness, or trouble speaking. Treat those as emergencies too.
What raises your risk — and what to do about it
Major risks include recent surgery, long bed rest, long flights or car rides, cancer, pregnancy, birth control pills or hormone therapy, smoking, obesity, and some inherited blood conditions. Age and a history of clots matter, too.
Simple prevention steps work well: move often on long trips, drink water, avoid smoking, and keep a healthy weight. If you’ve had surgery or will be immobile, your doctor may prescribe blood thinners or recommend compression stockings. Follow those instructions closely.
If a doctor suspects a clot, they may order a Doppler ultrasound for legs, a D-dimer blood test, or a CT pulmonary angiogram for the lungs. Treatment usually starts quickly with anticoagulants (blood thinners) such as heparin, warfarin, or newer direct oral anticoagulants like rivaroxaban or apixaban. In severe cases, clot-busting drugs or procedures may be used.
While taking blood thinners, watch for unusual bleeding (easy bruising, blood in urine or stools, or long nosebleeds) and tell your provider about any new medications or supplements — some increase bleeding risk. Don’t stop or change doses without checking with your clinician.
Practical travel tips: stand up and walk every hour, do calf stretches in your seat, wear loose clothes, and avoid alcohol on long flights. If you have a high risk, ask your doctor before travel.
If you’ve had swelling, shortness of breath, or unexplained pain, see a clinician sooner rather than later. Quick testing and treatment cut complications and lower the chance a clot causes lasting harm.
Want more? Check articles on leg swelling (oedema) or heart health (like statins) to learn how related conditions can change your risk. If you have questions about symptoms or meds, contact your healthcare provider promptly.
The Link Between Blood Clots and Heart Attacks
As a blogger, I recently came across some fascinating information about the link between blood clots and heart attacks. It turns out that blood clots are a significant cause of heart attacks, as they can block the flow of blood to the heart muscle. When this happens, it can lead to a heart attack, which can be life-threatening if not treated promptly. It's essential to be aware of the risk factors for blood clots, such as smoking, obesity, and a sedentary lifestyle, in order to take preventive measures. In conclusion, understanding the connection between blood clots and heart attacks can help us take better care of our cardiovascular health.