Easier Eating: Simple Tips, Low-Acid Meals, and Medication Advice
Struggling to eat without pain, heartburn, or nausea? This page gathers practical tips, meal ideas, and medicine-related advice to make eating easier day-to-day. You'll find low-acid recipe ideas, ways to manage swallowing or swelling problems, and how some drugs can change appetite or digestion.
Start with meals you can actually finish. Choose soft textures—stews, purees, oats, scrambled eggs, and smoothies with mild fruits like banana or melon. For reflux or GERD, low-acid choices matter: cooked vegetables, lean proteins like chicken or fish, rice, and non-citrus fruits. Avoid tomatoes, citrus, spicy sauces, and greasy fried foods that trigger burning.
Small, regular portions help. Eating five to six small meals keeps your stomach settled and cuts pressure that forces stomach acid up. Sit upright during and after food for 30–60 minutes; gravity helps keep food and acid down. Chew slowly and keep bites small to reduce bloating and make digestion easier.
Quick kitchen fixes
Make simple swaps: cook with olive oil instead of butter, use low-fat yogurt instead of cream, and skip raw onion or hot peppers. Add gentle flavor with herbs like basil, parsley, or dill. Baking, steaming, or poaching are kinder to sensitive stomachs than frying or grilling. Prep a batch of low-acid soups or grain bowls you can reheat for fast, safe meals.
For those with swollen ankles or general oedema, reduce salty processed foods and pick potassium-rich options like cooked spinach, bananas, and beans. Swelling can make standing to cook or eat painful—pick one-pot meals you can eat while seated or use a stool in the kitchen to save energy.
When meds affect your eating
Many common medicines change appetite, cause nausea, or alter taste. Antihistamines, painkillers like ketorolac, statins, and some antidepressants can make meals harder to enjoy. If a drug causes nausea, try taking it with a bland snack, or ask your doctor about splitting doses. Some meds need food for proper absorption—always check instructions.
If neuropathic pain drugs like gabapentin or pregabalin make you sleepy or reduce appetite, schedule meals when you feel most alert. For severe nausea, ask about alternatives such as antiemetics or dose adjustments. Never stop a prescribed drug without talking to your provider.
Use supplements carefully. Some herbal products help digestion, but they can interact with prescription meds. Tell your pharmacist about everything you take so they can flag interactions. For reflux, dietary changes and timing usually help more than over-the-counter fixes alone.
Want easy meal examples? Try a gentle oatmeal with mashed banana and almond milk, a baked white fish with steamed zucchini and rice, or a blended lentil soup with mild spices. Keep snacks like plain crackers, applesauce, or low-fat yogurt on hand when appetite dips.
If eating problems persist, see a doctor or dietitian to check for conditions like GERD, oesophageal issues, malabsorption, or medication side effects. Small changes often make eating more comfortable fast—and you don’t have to do them alone.
Want more practical help? Check our Low-Acid Diet Recipes post for seven easy meals and step-by-step cooking tips. Read articles on oedema, medication guides like Phenergan or ketorolac, and pain meds such as gabapentin to learn side effects that affect eating. If you're unsure which changes fit you, message a dietitian or your prescriber — they can tailor a plan that keeps meals tasty and safe.
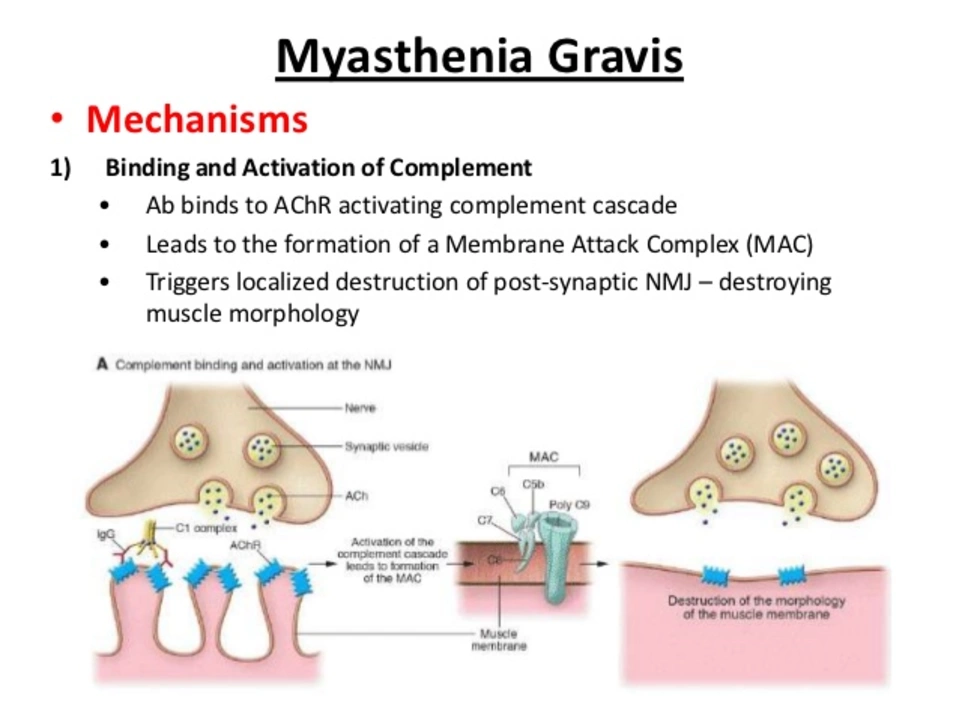
Myasthenia Gravis and Swallowing Issues: Tips for Easier Eating
In my recent blog post, I discussed the challenges faced by individuals with Myasthenia Gravis when it comes to swallowing and eating. I shared some useful tips that can make the process easier, such as opting for softer foods, eating smaller portions, and taking breaks during meals. Additionally, I emphasized the importance of maintaining proper body posture while eating and seeking professional help from speech therapists or dietitians if needed. Overall, my goal was to raise awareness and provide support for those struggling with this often overlooked aspect of living with Myasthenia Gravis.
- View More
- 17