Myasthenia Gravis: What to Watch For and What to Do
Feeling muscle weakness that gets worse after activity and better with rest? That’s the classic sign of myasthenia gravis, a condition where the immune system interferes with nerve-to-muscle signals. It often starts with droopy eyelids, double vision, or trouble chewing and speaking. Knowing the common signs helps you get care faster.
Common symptoms and warning signs
Look for these red flags: drooping eyelids, blurred or double vision, slurred speech, weak chewing, trouble swallowing, shortness of breath, and arms or legs that tire quickly. Symptoms usually vary day to day and often worsen as the day goes on. If breathing or swallowing becomes hard, treat it as an emergency and get immediate medical help.
How doctors diagnose myasthenia gravis
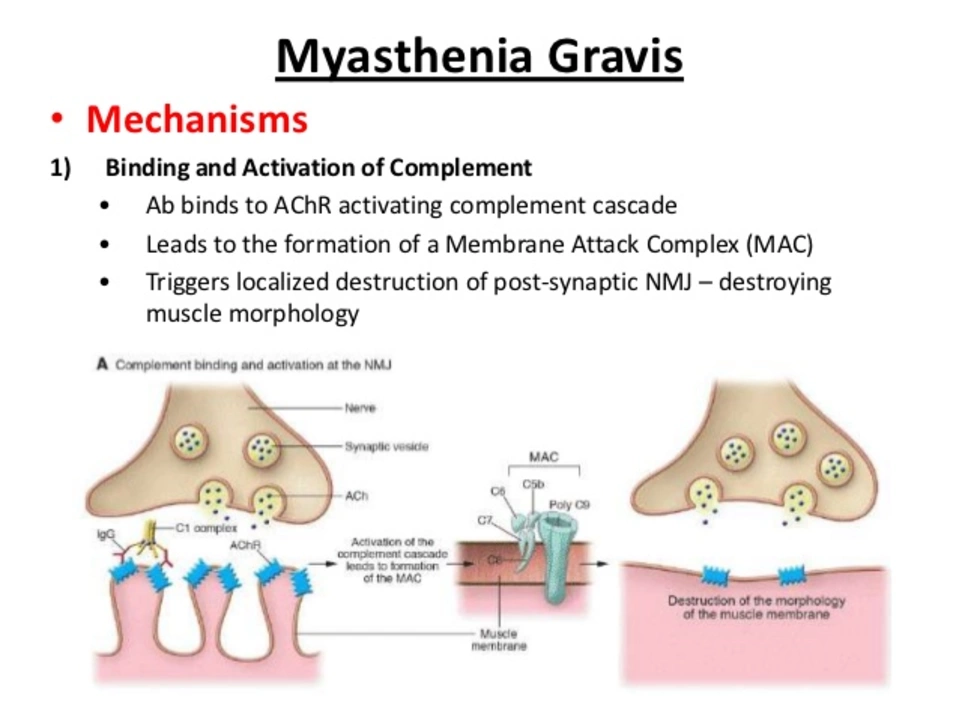
Diagnosis usually starts with a neurologist. They’ll do a focused exam to test muscle strength and how it changes with use. Common tests include blood tests for antibodies (AChR or MuSK), a nerve stimulation test, and sometimes a single-fiber EMG. A chest CT or MRI may be ordered to look for a thymoma (a tumor of the thymus), because the thymus is often linked to this illness.
Treatment choices depend on how severe symptoms are. For many people, pyridostigmine (an anticholinesterase) helps quickly by improving nerve signals to muscles. Steroids and other immunosuppressants (azathioprine, mycophenolate) calm the immune system over weeks to months. For fast, short-term control during bad episodes, IVIG or plasmapheresis can reduce symptoms in days to weeks.
Thymectomy — removing the thymus — is recommended for people with a thymoma and often considered for younger patients without a tumor. It can reduce symptoms or lower medication needs over time. Talk with your neurologist or surgeon about risks and expected benefit for your case.
Medications and everyday safety: some common drugs can make myasthenia worse, including certain antibiotics (like aminoglycosides), some heart meds, and strong sedatives. Always tell every provider, pharmacist, and dentist that you have myasthenia gravis so they can avoid risky drugs. Keep a list of safe and unsafe meds handy.
Daily life tips: pace activities, take naps, eat softer foods if chewing is hard, and use adaptive tools (long-handled utensils, shower chairs). If you drive, check vision and muscle control first. Small changes often make a big difference in energy and safety.
Mental and social support matter. Fatigue and uncertainty can be stressful — join a support group or talk to others with myasthenia gravis. Your care team can connect you with local resources and rehab specialists who help with swallowing, speech, and physical conditioning.
Want more specific info or articles on related meds and treatments? Browse trusted resources and always confirm treatment choices with your neurologist. Myasthenia gravis is manageable for many people with the right plan and timely care.
Myasthenia Gravis and Swallowing Issues: Tips for Easier Eating
In my recent blog post, I discussed the challenges faced by individuals with Myasthenia Gravis when it comes to swallowing and eating. I shared some useful tips that can make the process easier, such as opting for softer foods, eating smaller portions, and taking breaks during meals. Additionally, I emphasized the importance of maintaining proper body posture while eating and seeking professional help from speech therapists or dietitians if needed. Overall, my goal was to raise awareness and provide support for those struggling with this often overlooked aspect of living with Myasthenia Gravis.
- View More
- 17