Sinus infections: what to watch for and how to treat them
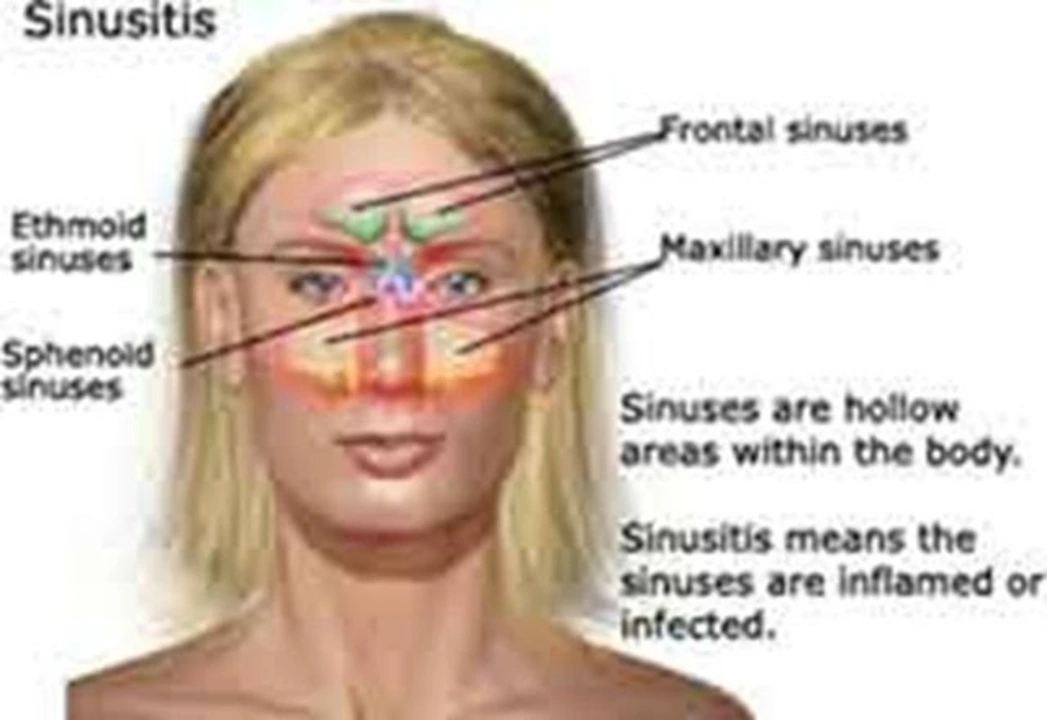
Got a blocked, painful face and thick green mucus that won’t quit? That could be a sinus infection (sinusitis). It often follows a cold and can feel worse than a regular runny nose—pressure around the forehead, cheekbones, or behind the eyes, reduced smell, sore throat, and sometimes fever.
Sinus infections come in two common types: acute (short, often follows a cold) and chronic (symptoms that last 12 weeks or more). Acute cases often clear up with home care; chronic ones usually need a medical plan and sometimes tests to find the cause.
Quick self-care steps that help right away
Start simple and practical. Use saline nasal rinses (a neti pot or squeeze bottle) twice daily to flush mucus and ease pressure. Warm compresses over the face for 10–15 minutes can relieve pain. Running a humidifier or taking hot showers helps thin mucus and makes breathing easier.
Over-the-counter options: plain saline sprays, ibuprofen or acetaminophen for pain, and short-term oral decongestants if you don’t have high blood pressure. Guaifenesin (an expectorant) can loosen thick mucus. If allergies trigger your symptoms, a non-drowsy antihistamine or a steroid nasal spray (used regularly) often reduces inflammation.
Be careful with nasal decongestant sprays—they help for a few days but can cause rebound congestion if used more than 3 days.
Medical treatments and when to see a doctor
Most viral sinus infections improve within 7–10 days. See a doctor if symptoms get much worse after 5–7 days, persist beyond 10 days without improvement, or you have a high fever, severe facial pain, swelling around the eye, or repeated infections. Those signs may mean a bacterial infection, a complication, or an underlying issue like a deviated septum or nasal polyp.
Doctors decide on antibiotics only when a bacterial infection is likely. If prescribed, finish the course. For chronic or recurrent cases, your doctor may recommend nasal steroid sprays, longer saline rinses, allergy testing, or ENT referral for imaging and possible procedures.
If you’re using prescription meds, buy from licensed pharmacies and confirm the product and dose. On CanadaDrugsDirect.com you’ll find trusted info on common medications and safe ways to manage prescriptions in Canada.
Watch for red flags: severe headache, vision changes, confusion, or neck stiffness need urgent care. For most people, simple steps—saline rinses, steam, rest, and targeted meds—are enough to feel better within a week or two.
If symptoms keep coming back, ask your doctor about longer-term solutions like allergy control, sinus imaging, or ENT evaluation. Small changes—humidity in winter, quitting smoking, and managing allergies—cut down repeat infections a lot.
The Connection Between Fever and Sinus Infections
As a blogger, I've recently looked into the connection between fever and sinus infections. I've discovered that fevers are often a sign that our body is fighting an infection, such as a sinus infection. Sinus infections, or sinusitis, occur when the cavities around our nasal passages become inflamed, leading to symptoms like congestion, facial pain, and fever. It's important to recognize these symptoms and seek medical help if needed as prolonged sinus infections can lead to more severe complications. In summary, fever is a common symptom of sinus infections and indicates that our body is working to fight off the infection.
- View More
- 19