Spirometry: What It Is, Why It Matters, and How It Guides Lung Health
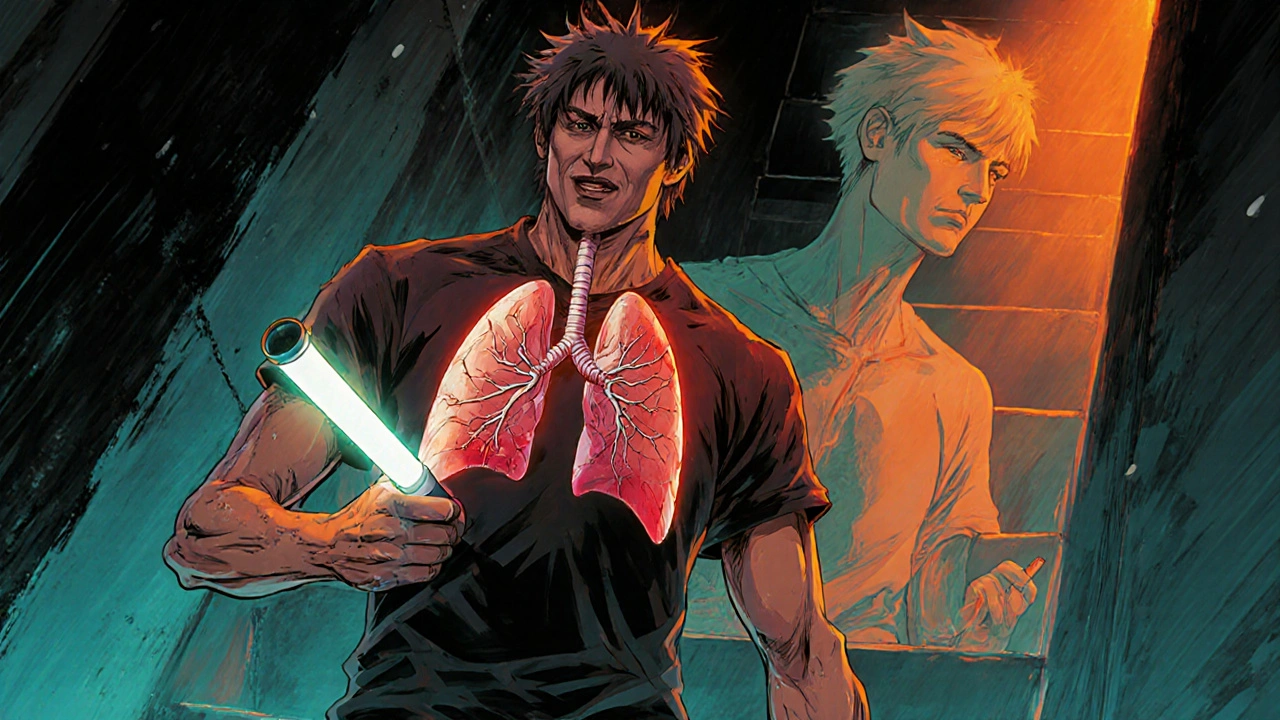
When your doctor suspects you have a breathing problem, they often start with a spirometry, a simple, non-invasive lung function test that measures how much air you can breathe in and out, and how fast you can do it. Also known as a pulmonary function test, it’s one of the most common and reliable tools doctors use to spot problems like asthma, COPD, or even early lung damage from smoking or pollution. Unlike X-rays or blood tests, spirometry gives real-time data on how your lungs are actually performing—no needles, no radiation, just you breathing into a tube.
This test isn’t just for people with symptoms. If you’re a smoker over 40, work around dust or chemicals, or have a family history of lung disease, spirometry can catch trouble before it gets serious. It’s also used to track how well treatments like inhalers or oxygen therapy are working. The numbers it produces—like FEV1 and FVC—are not just numbers; they’re clues that tell your doctor whether your airways are narrowed, your lungs are stiff, or your breathing muscles are weakening. And because these values change over time, spirometry helps decide if you need to adjust your meds, quit smoking, or start pulmonary rehab.
It’s not just about asthma and COPD. Spirometry plays a role in preparing for surgery, checking for occupational lung diseases, and even evaluating unexplained shortness of breath in athletes or older adults. You’ll find posts here that connect spirometry to real-world decisions: how results affect medication choices, why some people skip the test even when they should, and how insurance or workplace health programs handle it. You’ll also see how it ties into other tests like blood oxygen levels, chest X-rays, and even heart function markers like NT-proBNP—because lung and heart health are deeply linked.
What you’ll find below isn’t a list of medical jargon. It’s a collection of clear, practical guides written by people who’ve been through this—whether they’re patients managing chronic lung disease, caregivers helping aging parents, or workers exposed to lung irritants. These posts don’t just explain spirometry—they show you what to do with the results, how to talk to your doctor about them, and when to push for more answers. You’ll learn how lung function tests fit into bigger health stories: from gout meds affecting breathing to fiber supplements interfering with inhalers, and how generic drug pricing impacts access to the tools you need to monitor your lungs.
COPD Explained: Understanding Disease Stages and Effective Treatment Options
COPD is a progressive lung disease with four stages, from mild to very severe. Learn how spirometry determines your stage, what treatments work at each level, and how to slow progression. Early action saves breath - and life.
- View More
- 17