Understanding Chronic Obstructive Pulmonary Disorder (COPD)
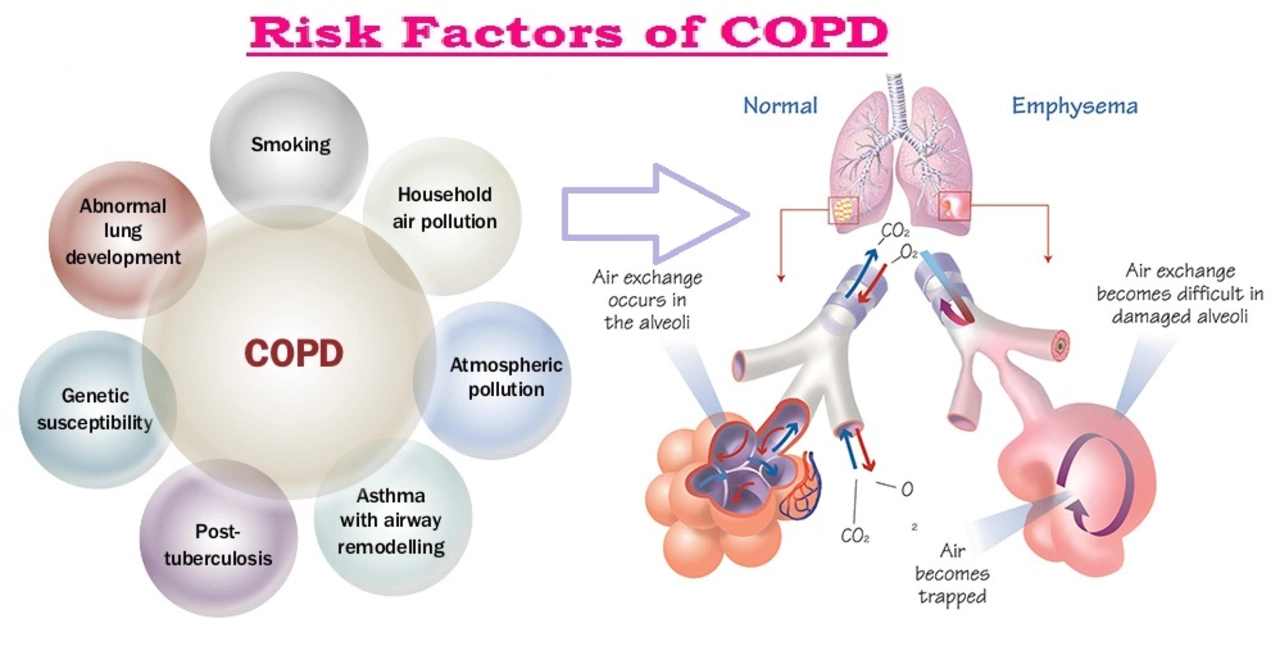
Before diving into the impact of Chronic Obstructive Pulmonary Disorder (COPD) on work and employment, let's first understand what COPD is. COPD is a chronic lung disease that affects millions of people worldwide. It is characterized by progressive airflow limitation, which makes it increasingly difficult to breathe over time. The two main types of COPD are chronic bronchitis and emphysema, both of which cause inflammation and damage to the airways and lungs.
As a person living with COPD, it is essential to be aware of how this condition can affect various aspects of your life, including your ability to work and maintain employment. In this article, we will discuss the impact of COPD on work and employment, and provide guidance on how to manage these challenges and maintain a fulfilling professional life.
COPD Symptoms Interfering with Work Performance
One of the primary ways COPD impacts work and employment is through the symptoms it causes. These symptoms, which include shortness of breath, chronic cough, and fatigue, can make it difficult to perform physical tasks and maintain focus throughout the workday. For instance, if your job requires you to climb stairs or lift heavy objects, you may find it increasingly difficult to complete these tasks as your COPD progresses. Additionally, the constant coughing and fatigue associated with COPD can be distracting, making it hard to concentrate on your work and stay productive.
It is essential to communicate with your employer about your condition and any limitations you may have due to your COPD. This open communication can help create a more understanding and supportive work environment, and your employer may be able to make accommodations to help you maintain your job performance.
Managing COPD in the Workplace
There are several strategies you can employ to manage your COPD symptoms in the workplace. First and foremost, it is crucial to follow your doctor's recommendations and take your prescribed medications as directed. This will help manage your symptoms and slow the progression of your COPD.
Additionally, consider making some adjustments to your work environment to help minimize the impact of your COPD symptoms. For example, if possible, try to minimize your exposure to irritants like dust, chemicals, and smoke, which can exacerbate your symptoms. You may also consider requesting a more ergonomic workstation or using a portable fan to improve air circulation around your workspace.
Lastly, be sure to practice good self-care, including maintaining a healthy diet, getting regular exercise, and prioritizing sleep. These habits will not only benefit your overall health, but they can also help manage your COPD symptoms and improve your ability to work.
Legal Protections and Accommodations for Employees with COPD
If you are an employee with COPD, it's essential to be aware of the legal protections and accommodations that may be available to you. In many countries, including the United States, laws such as the Americans with Disabilities Act (ADA) protect employees with disabilities, including those with COPD, from discrimination and require employers to provide reasonable accommodations to help them perform their job duties.
These accommodations may include flexible work schedules, additional break times, telecommuting options, and modifications to the work environment, such as improved air quality or ergonomic workstations. To request accommodations, you will need to disclose your COPD diagnosis to your employer and provide documentation from your healthcare provider outlining your limitations and recommended accommodations.
Remember, it is your right to request and receive reasonable accommodations to help you manage your COPD symptoms in the workplace. Do not hesitate to advocate for yourself and your needs to ensure a supportive and accommodating work environment.
Considering a Career Change for Better COPD Management
As your COPD progresses, you may find that your current job is no longer suitable for your physical abilities and health needs. In such cases, it may be necessary to consider a career change or transition to a less physically demanding role within your current company. This can be a challenging decision to make, but it is essential to prioritize your health and well-being above all else.
When considering a career change, think about your skills, interests, and passions, and look for opportunities that align with your abilities and health needs. You may also want to consult with a career counselor or vocational rehabilitation specialist who can help you explore your options and provide guidance on transitioning to a new career that better accommodates your COPD.
In conclusion, living with COPD can indeed present challenges in the workplace, but by understanding your rights, advocating for yourself, and making necessary adjustments, you can continue to have a fulfilling professional life. Remember to communicate openly with your employer, practice good self-care, and consider all available options to help you manage your COPD while maintaining your employment.




COPD sucks.
It is a matter of public health that modern workplaces remain indifferent to pulmonary disease. The relentless demand for productivity forces workers to inhale hazardous fumes without recourse. One ought to recognize that the legal safeguards exist, yet enforcement is often lax. Therefore, advocacy is essential for those battling chronic breathlessness.
Managing COPD at work calls for a blend of self‑advocacy and pragmatic adjustments. Employees should seek ergonomic solutions and negotiate flexible schedules to preserve stamina. Employers benefit when they retain experienced staff through reasonable accommodations. Mutual respect paves the way for sustained productivity.
Chronic obstructive pulmonary disease presents a multifactorial challenge within occupational health frameworks, intersecting physiological decline, psychosocial stressors, and regulatory compliance. First, the pathophysiology of airflow limitation translates into reduced aerobic capacity, which directly impairs performance of both manual and sedentary tasks. Second, symptom fluctuations-particularly episodic dyspnea and nocturnal cough-create unpredictable work attendance patterns that strain staffing models. Third, exposure to occupational irritants such as silica dust, volatile organic compounds, and tobacco smoke accelerates disease progression, thereby tightening the feedback loop between environment and health. Fourth, the legal landscape, epitomized by statutes like the Americans with Disabilities Act, obligates employers to implement reasonable accommodations, yet the interpretive burden often falls on the employee to document functional limitations. Fifth, occupational therapists and pulmonary rehabilitation specialists can devise work‑specific conditioning programs that enhance inspiratory muscle strength and endurance, mitigating functional loss. Sixth, assistive technologies-including portable nebulizers, supplemental oxygen delivery systems, and air‑purifying devices-can be integrated into the workstation to maintain ambient air quality. Seventh, organizational culture that fosters open communication reduces stigma and encourages timely disclosure of health needs. Eighth, human resources policies that incorporate progressive leave options and telecommuting provisions align with the chronic nature of COPD, allowing workers to manage exacerbations without jeopardizing job security. Ninth, interdisciplinary collaboration among physicians, occupational health nurses, and safety officers ensures that risk assessments are updated in response to evolving clinical status. Tenth, data analytics from wearable spirometry can inform predictive scheduling, enabling proactive workload redistribution during periods of heightened symptom burden. Eleventh, employee assistance programs that offer counseling address the psychological sequelae of living with a progressive illness, thereby preserving mental resilience. Twelfth, continuous education for managers on disease awareness improves accommodation decision‑making. Thirteenth, fiscal analyses reveal that investment in accommodation and preventive measures often offsets costs associated with turnover and absenteeism. Fourteenth, peer support networks within the workplace facilitate shared coping strategies and reinforce adherence to treatment regimens. Fifteenth, legislative advocacy remains crucial to expand coverage of pulmonary disease under occupational safety statutes. Ultimately, a comprehensive, evidence‑based approach that integrates clinical management, ergonomic adaptation, legal compliance, and psychosocial support can transform COPD from a career‑limiting condition into a manageable occupational factor.
You've covered the terrain brilliantly, and it's clear that a systematic plan can make a real difference for anyone dealing with COPD. In practice, start by requesting a formal accommodation meeting and bring your latest pulmonary function report. Pair that with a simple home‑exercise routine-like diaphragmatic breathing and low‑impact cardio-to keep your lungs as strong as possible. Remember, consistent follow‑up with your respiratory therapist will fine‑tune your workplace modifications over time.
Not every COPD case requires a career overhaul; many can stay in their current roles with modest tweaks.
While it's true that minor adjustments often suffice, we must also acknowledge that disease severity varies widely, and some individuals genuinely need a different environment to thrive.
Great points, especially the emphasis on clear documentation 😊. A solid paper trail makes the accommodation request smoother.
Sending lots of love to anyone juggling COPD and a job 💙. Small victories like finding a comfortable chair or a quiet corner can add up to big improvements in daily comfort.
It's unacceptable that anyone has to compromise their health for a paycheck. Employers must view health accommodation as a moral imperative, not a charitable favor.