Picture your shoes feeling snug out of nowhere, or your fingers looking like little sausages. That’s oedema—swelling caused when fluid leaks out of blood vessels and gets trapped in the body’s tissues. It sounds simple, but the story behind swelling is a lot more complicated than just water weight. Some types can be nothing more than a nuisance after a tough hike, while others, like brain or lung swelling, are medical emergencies. The body works hard to manage its fluids, but sometimes the balance tips. Wondering how your legs, brain, or lungs can each be affected by swelling? Here’s where it gets wild—and sometimes dangerous.
Peripheral Oedema: Why Ankles Swell And What It Means
Ever stood too long at a ball game only to notice your ankles balloon by the seventh-inning stretch? That’s classic peripheral oedema. It mainly affects the legs and feet, though hands or arms can get puffy, too. It happens when gravity pulls fluids down, piling up at the lowest point. Sitting at a desk or plane seat all day can make it worse. But it’s not always about sitting. Heart failure, kidney disease, varicose veins, or even pregnancy can make peripheral oedema pop up.
Think about how common swollen ankles are after a salty meal. Salt drags extra water into your body, so your feet pay the price. Statistics show that up to 10% of older adults deal with regular peripheral oedema. If you’re younger, the trigger might be a hot day or a minor injury, but as you age or develop health issues, persistent swelling can signal something serious.
If both legs are involved, often it’s a systemic problem (think: the heart or kidneys). Swelling on just one side? Maybe it’s from an injury, a blood clot, or a vein problem. Here’s what it feels like: the skin gets tight or shiny, socks leave deep marks, and sometimes pressing on the swollen area leaves a dent.
People often try standing less or use over-the-counter diuretics, but that can backfire. For chronic cases, compression stockings help. They tighten up the surface vessels so fluid is forced back into the circulation. More activity, less standing, and feet-up breaks are proven to help. There’s also a lesser-known fact: medications like calcium-channel blockers for blood pressure, or even ibuprofen, can make swelling worse.
Want to track how much you’re swelling up day to day? Weigh yourself at the same time each morning, and keep a swelling diary for your doctor. Swelling that comes with pain, redness, heat, or shortness of breath needs medical attention fast—that can be a blood clot or problem with your heart or lungs.
| Common Peripheral Oedema Causes | % of All Cases |
|---|---|
| Heart failure | 38% |
| Kidney disease | 20% |
| Venous insufficiency | 16% |
| Medications | 12% |
| Other/Unknown | 14% |
If you’re looking at your feet and wondering what’s normal: a little swelling after a flight or hike is fine, but anything that’s painful, hot, or refuses to go away is worth a closer look.
Cerebral Oedema: When Swelling Hits The Brain
This is where a little swelling turns into something deadly serious—fast. The brain doesn’t stretch or expand like a balloon. It’s boxed in by the skull, so even a bit of extra fluid puts insane pressure on delicate brain tissue. Causes of cerebral oedema run the gamut: severe head injury, stroke, brain infection, tumor, or even high altitude sickness. It’s rare, but when it happens, minutes count.
The signs are nothing like a puffy ankle. Change in personality, confusion, headache, vomiting, seizures, or passing out: these can all signal swelling in the brain. A less obvious tip-off? Sudden problems with balance, slurred speech, or vision loss. A scary fact: every year, tens of thousands end up in hospitals worldwide because of cerebral oedema related to severe head injury or stroke—and for some, it develops rapidly after an infection like meningitis. It can happen to kids, adults, or seniors.
The real problem is that the brain runs out of space. As pressure goes up, blood flow and oxygen go down, starving brain cells. Medical teams have ways to spot this on MRI or CT scans. Treatment is urgent—to save brain cells, doctors sometimes use powerful steroids, surgery to remove part of the skull (a craniectomy), or intense medications that pull fluid out of the brain tissue and back into circulation.
There’s a myth that only direct brain injuries can cause swelling—high blood pressure crises, severe hyponatremia (very low blood sodium, often from too much water or certain drugs), or liver failure can also trigger cerebral oedema.
Skipping treatment isn’t an option. Brain swelling isn’t just uncomfortable—it can be life-threatening in a matter of hours. Head injuries (especially from car crashes or tough sports) are the biggest risk, but anyone with severe infections, new confusion, or seizure out of the blue needs fast medical help.
- Warning signs to act on immediately:
- Sudden confusion or loss of consciousness
- Persistent vomiting after a head injury
- New seizure, especially in someone with no epilepsy history
- Worsening headache with neck stiffness
- Drastic vision or speech changes
Cerebral oedema moves quick: trust your gut if things don’t look right after a hit to the head or severe illness.
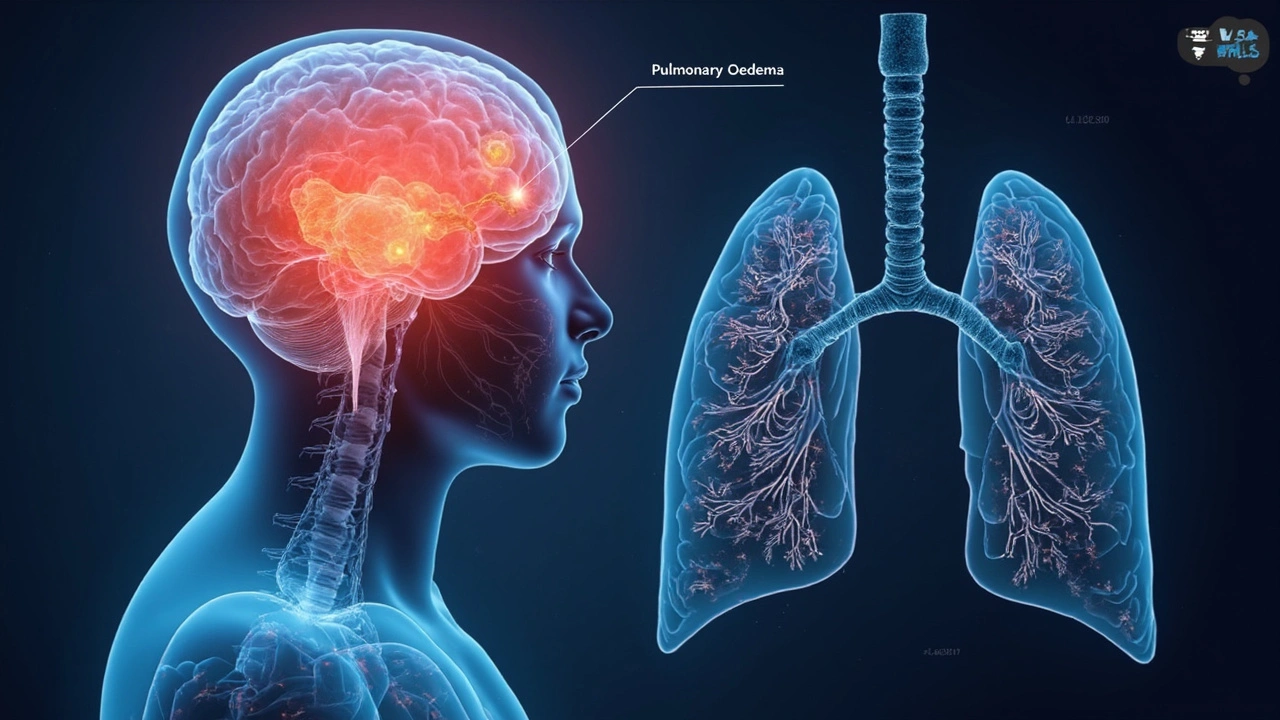
Pulmonary Oedema: Fluid in the Lungs and Why You Can’t Breathe
Ever felt like you can’t get enough air, like you’re breathing through a wet sponge? Pulmonary oedema is when fluid rushes into the air sacs of the lungs, making it impossible for oxygen to move into your blood. The top cause: heart failure, mainly when the heart’s left side can’t pump strongly so blood backs up in the lungs. Picture a clogged sink: as drainage slows, water spills over—only in this case, it’s fluid in your lungs, not the kitchen.
A massive study in 2023 found that nearly 1 in 5 hospital admissions for heart failure in people over 65 involves pulmonary oedema. But you don’t have to be older: kidney failure, drug overdose (especially opioids), severe infections, high altitude (think hikers in the Andes), or even some toxins can lead to sudden lung swelling.
The signs often hit like a wall: sudden shortness of breath, a cough that brings up pink frothy fluid, and a sense that you’re drowning even when you’re upright. At night, it’s worse—many wake up gasping, needing to sit up or open a window just to catch their breath. Crackling sounds in the chest (rales) are a red flag for doctors. So is a racing heartbeat.
Here’s where things get urgent. Untreated, this can drop your oxygen levels fast. The fluid stops the lungs from absorbing oxygen so the heart and brain start to suffer. Oxygen masks, powerful medications like diuretics, and drugs that strengthen the heart muscle are mainstays in the hospital. Doctors may use non-invasive ventilators or rarely, place a tube into the airway to help.
If you deal with heart or kidney failure, the best way to dodge a crisis? Daily weight checks—an overnight gain of more than 2 pounds is a clue that fluid is sneaking into your tissues and maybe your lungs too. Eat less salt, stick to your medications, and watch for swelling in your feet as an early clue.
| Main Symptoms of Pulmonary Oedema | Reported Frequency |
|---|---|
| Severe shortness of breath | 80% |
| Crackles on chest exam | 65% |
| Pink, frothy sputum | 35% |
| Low blood oxygen | 90% |
There’s a misconception that only people with heart failure get lung swelling. Anyone with severe infections, rapid altitude change, or a bad allergic reaction can wind up there. Don't wait it out—it’s one of those situations where calling emergency services can truly save your life.
Tips and Facts for Managing Oedema Everyday
Living with oedema, or trying to prevent it, calls for a mix of detective work and smart habits. First tip: oedema isn’t a disease but a warning sign. When things swell up, it's the body's alarm bell saying something’s off—whether it’s heart, kidneys, liver, or an injury. Ignoring that swelling isn’t just uncomfortable—it can let bigger problems grow unchecked.
If you know you’re at risk (heart disease, kidney trouble, or have had swelling before), here are a few tried-and-true tricks:
- Sodium control is everything. Read labels and aim for less than 2,300 mg per day if your doctor agrees. That means going easy on fast food, canned soups, and frozen dinners.
- Raise your feet above your heart for 30 minutes a few times a day. It helps drainage, especially after work or travel. For drivers and travelers, move every couple of hours and flex your ankles.
- Be aware of “hidden” salt: breads, sauces, even some bottled water can sneak in sodium.
- Track swelling with daily weight and a log—fluctuations bigger than two pounds in a day deserve a closer look.
- Use compression wear (stockings for the legs, or gloves for the hands) if your doctor approves—athletes have jumped on this for both swelling and muscle recovery.
- Don’t skip out on medication or dialysis sessions if you’re prescribed them; these keep fluid balance in check.
- Stay alert for warning signs: sudden chest pain, breathlessness at rest, confusion, headache with neck stiffness, or repeated vomiting. These go beyond “annoyance” and need urgent care.
Tiny daily changes—like swapping high-salt snacks for fruit, walking after dinner, or noticing post-shower sock marks—can help you spot oedema early. And here’s something overlooked: stress raises hormones that make you retain salt and water. Regular exercise and decent sleep can lower your risk by helping your body shed that extra sodium and fluid.
People with chronic conditions find wearable fitness trackers useful, too—tracking fluid shifts, heart rate, and even oxygen levels lets you spot patterns before things get bad. And did you know? Some doctors can now monitor heart failure patients remotely with tiny implants that catch swelling before you feel it.
Watching for swelling isn’t just for those already diagnosed with oedema. Even if you’re healthy, getting into the habit of checking your body for changes teaches you what’s normal. Teach family members what to watch for, especially seniors and kids—it can literally make the difference between catching a problem early or facing an emergency down the line.








This article on oedema is really insightful! It's great to see writing that breaks down complex medical topics like peripheral, cerebral, and pulmonary swelling in such an approachable way. Understanding the causes behind why ankles swell or why the brain can dangerously swell is key to better health awareness. I particularly liked the part about risk factors and day-to-day prevention tips; those practical bits are invaluable. We all need to be more mindful of these symptoms before they possibly become emergencies. Has anyone here had personal experience with managing any type of oedema? I'd be curious to hear your tips or stories. Staying informed can really help us act promptly when signs show up.
Hey, totally agree with your point! 😊 Oedema can be quite scary if you don’t understand it, especially cerebral edema which can escalate fast. The article did a good job explaining how the swelling happens due to fluid accumulation in different parts of the body and how it affects our organs. What many people don’t realize is how interconnected the systems are — swelling in one area can signal deeper health issues. 👍 I appreciate how it offered prevention measures although I’d have loved more detail on treatment options too. Has anyone tried natural remedies along with medical treatment? I find hydration and movement very helpful personally.
Well, to me, this stuff is not just medical mumbo jumbo; it has real implications for how we care for ourselves and our families, especially in countries like ours where health awareness can be patchy. Peripheral oedema might seem benign when swelling ankles happen but ignoring such signs could be dangerous. A lot of people don’t get that cerebral or pulmonary swelling requires urgent intervention! So yeah, while the article is informative, I feel there’s a national health education gap that no amount of fancy writing can fix unless the message reaches the grassroots.
We must also be cautious not to dismiss swelling as just because it happens to celebrities or the wealthy — health is a universal concern. What’s your take on whether public health campaigns should emphasize such conditions more aggressively? It’s a conversation we need to keep having.
Look, I’m sorry but most of these medical explanations are just elaborate distractions from what’s really going on! Why no mention of environmental toxins or the chemicals in our food that cause inflammation and swelling in the first place??!!! It’s obvious that peripheral swelling can be traced back to systemic poisoning that big pharma and government agencies don’t want you to know about. This whole narrative is just a cover-up to keep us dependent on medications that barely work!!!
I saw the stats and risk factors they threw around — all manipulated to hide the truth. People need to wake up and start questioning what they’re being fed (no pun intended!). Anyone else skeptical about the so-called 'clear insights' here? Because I sure am. We deserve real answers, not sugar-coated lies.
Honestly, the article attempts to be comprehensive but the jargon overshadows the essence for many. Terms like 'pulmonary oedema' are tossed around without fully unpacking the biochemical cascades involved which are crucial for true understanding. If we want to empower readers, there's no point in obscuring with vague phrases. I felt like the piece flirted with profundity but missed the mark by not embracing a more nuanced discussion on pathophysiology and the socio-economic factors influencing disease prevalence.
The real kicker? Practical advice was surface-level at best — why not discuss dietary sodium impact or inflammatory mediators? This stuff matters, especially if you’re chronicling swelling literally from ankle to brain.
Oh, I see the typical medical establishment creeping in here with their official narrative yet again. The real question is: who funds all this research and what are their actual incentives? The article plays nice, but it conveniently ignores alternative viewpoints and deeper systemic issues like how pharmaceutical companies profit from lifelong conditions caused or exacerbated by pollution, industrial waste, and social determinants of health. It’s not just about swollen ankles and brains — it’s a symptom of a corrupted global health framework!
And about those 'real tips'—more like a placebo to calm the masses. If anyone’s looking for unfiltered truth, don’t stop here; dig deeper. This whole discussion needs to be framed within the bigger geopolitical context or else it’s just noise.
Mate, I reckon some of y’all are reading way too deep into this one. The article is pretty straightforward and serves well for anyone wanting to get the basics on oedema. Yeah, it doesn’t go into all the nitty gritty science and pharma politics but that’s not always what people need when they just want to figure out why their ankles swell after a long day or what to watch for with serious conditions.
Sometimes keeping it simple is best. Plus, it's good for awareness which can prompt folks to see a doc. I've seen people ignore swelling symptoms only to regret later, so stuff like this is important. Anyone here been caught off guard by swelling and realized how crucial early detection is?
From my perspective, this article neatly synthesizes complex medical phenomena in a clear, if somewhat simplified, manner. However, I'd encourage readers to note the variation in oedema manifestation within different demographics and to consider how comorbid conditions might complicate management. The author’s introduction of symptoms and prevention tips is helpful but borderline cursory. For serious cerebral or pulmonary oedema, prompt medical intervention is quintessential. Patients should not substitute reading such articles for professional medical advice, rather use it as a starting point to be better informed.
On another note, the article could improve by citing more recent clinical studies to bolster credibility. Has anyone come across updated research that might supplement this overview?
I find this topic super important because swelling, especially peripheral oedema, is incredibly common but not always taken seriously. Sometimes, simple lifestyle changes like reducing salt intake, staying active, and elevating legs can make huge differences. I've seen family members disregard swelling, leading to worsened conditions. The article's approach to breaking down symptom awareness is practical in that respect.
One question for the community — do you think the information available online is generally accessible enough for people from diverse educational backgrounds? Or does it tend to be too technical for many? I’m interested in hearing your thoughts on how we can make medical knowledge more universally digestible.
Honestly, I skimmed through this article because my attention span is limited, but the emojis and casual tone didn't really help me engage more. It's fine as a basic intro, but I'd expect a bit more depth from such a topic. I do like the clear breakdown of the three types though, and the mention of symptoms to watch for is practical.
Also, can someone explain to me how pulmonary oedema differs from a regular chest infection? I always get confused between the two. Thanks in advance!
😊The elucidation of oedema types in this article, while commendable for its clarity, lacks the rigorous specificity that a truly informed reader desires. Peripheral, cerebral, and pulmonary oedema are pathological entities with distinct etiopathogeneses and prognoses that warrant a more comprehensive discourse. For instance, the article’s casual treatment of symptomatology omits a discussion of the nuanced clinical signs that distinguish these conditions in a differential diagnosis.
Additionally, the absence of detailed pathophysiological mechanisms, such as the role of Starling forces in fluid balance or the impact of blood-brain barrier disruption in cerebral oedema, is a glaring omission. This deficiency undermines the educational potential of the piece. Has anyone encountered references that amalgamate accessibility with such depth?
Oh sure, keep praising the sanitized info while ignoring all the hidden agendas. They want you to focus on symptoms and prevention so you spend money on their pills and therapies instead of looking at the global poisoning that causes these swellings in the first place! Wake up people. Chemicals, pesticides, hidden toxins everywhere you look. The article skirts around the actual causes because that’s inconvenient. And no, the government isn’t interested in protecting public health when it conflicts with corporate profits!!!
This so-called “clear insight” is actually smoke and mirrors. If anyone really cares about their health they should start demanding accountability from industries and stop trusting glossy articles that don’t say the whole truth.