Most people with chronic kidney disease (CKD) don’t know they have it-until it’s too late. By the time symptoms like fatigue, swelling, or foamy urine show up, the kidneys have already lost much of their function. But here’s the truth: chronic kidney disease can be caught early, and when it is, progression can often be stopped-or at least slowed down significantly. This isn’t theoretical. It’s backed by data, guidelines, and real patient outcomes.
What Chronic Kidney Disease Really Means
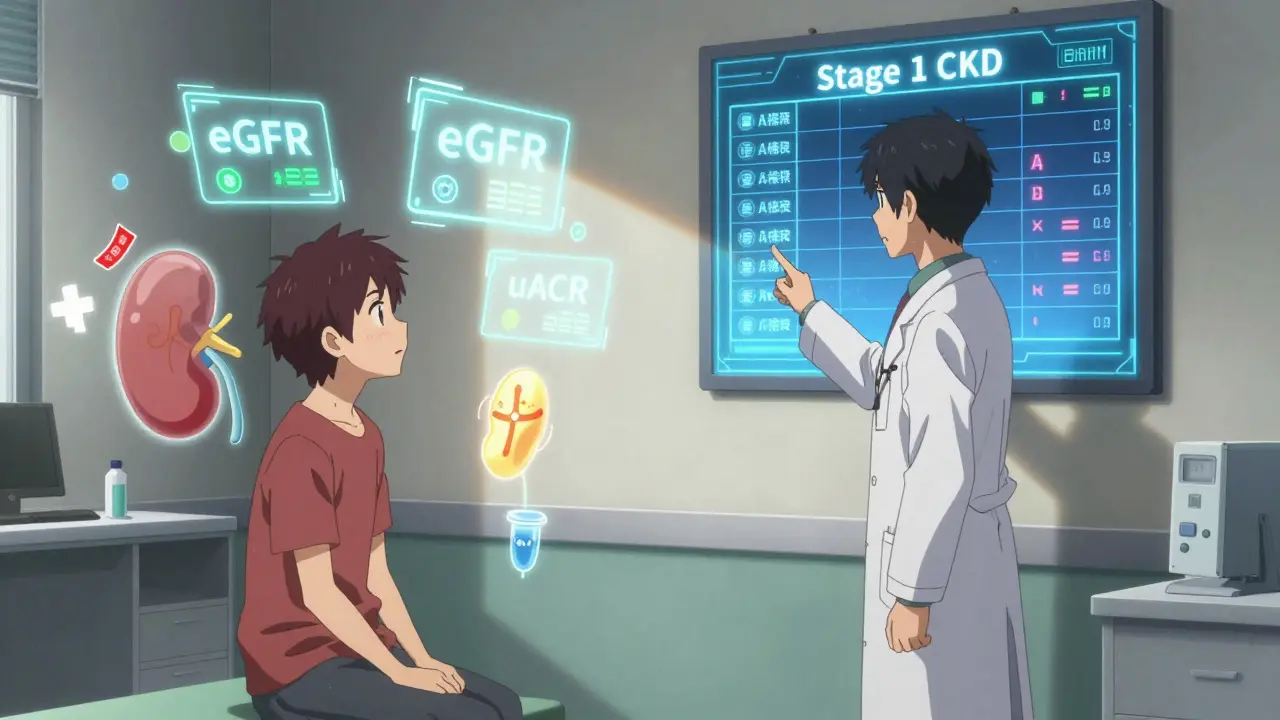
Chronic kidney disease isn’t just about high creatinine or a single lab result. It’s defined by two things: reduced kidney function lasting at least three months, or signs of kidney damage. That damage could show up as protein in your urine, blood in your urine, abnormal structure on an ultrasound, or other markers. The key word is chronic. One bad test doesn’t mean you have CKD. Two abnormal tests, three months apart, do. The current system, used worldwide since 2012, divides CKD into five stages based on your eGFR (estimated glomerular filtration rate) and whether you have kidney damage. Stage 1 is the mildest: eGFR above 90, but with protein in your urine. Stage 5 is kidney failure-when you need dialysis or a transplant. The scary part? Most people with Stage 1 or 2 CKD never get diagnosed. Why? Because doctors often only check one thing: serum creatinine. And that’s not enough.The Two Tests That Matter
If you’re at risk for kidney disease, you need two tests-not one. The first is eGFR. It’s calculated from your blood creatinine level, but it also factors in your age, sex, and race. The standard formula now is the CKD-EPI equation, which replaced older, less accurate versions. But creatinine alone is flawed. It can be normal even when your kidneys are damaged, especially if you’re older, have low muscle mass, or are a woman. That’s why the second test is non-negotiable: the urine albumin-to-creatinine ratio, or uACR. This simple, cheap test measures how much protein (albumin) is leaking into your urine. A value of 30 mg/g or higher means kidney damage is present. The American Diabetes Association, the National Kidney Foundation, and the KDIGO guidelines all agree: you need both tests to diagnose early CKD. Think of it like this: eGFR tells you how well your kidneys are filtering. uACR tells you if they’re leaking. One without the other is like checking only the oil light on your car and ignoring the check engine light. You might think everything’s fine-until the engine blows.Who Should Be Screened
Not everyone needs annual kidney tests. But if you fall into one of these groups, you should be screened every year:- People with type 1 or type 2 diabetes
- People with high blood pressure
- Those with a family history of kidney failure
- African Americans, Native Americans, and Hispanic individuals (who have 2 to 4 times higher risk)
- People over 60
- Those taking long-term NSAIDs (like ibuprofen), certain antibiotics, or other kidney-toxic drugs

Why Early Detection Works
Here’s where it gets powerful. If you catch CKD at Stage 1 or 2, you have a 5- to 7-year window to act. And the interventions? They’re simple, proven, and often covered by insurance. Medication: SGLT2 inhibitors (like dapagliflozin or empagliflozin), originally developed for diabetes, reduce the risk of kidney failure by 32% in people with albuminuria-even if they don’t have diabetes. ACE inhibitors and ARBs are also frontline drugs for lowering blood pressure and reducing protein leakage. Blood pressure control: Keeping your BP below 130/80 mmHg cuts progression risk by 27% compared to the old target of 140/90. That’s not a small difference-it’s life-changing. Diet and lifestyle: Reducing salt intake, losing excess weight, quitting smoking, and avoiding processed foods can slow eGFR decline from 3.5 mL/min/year to just 1.2 mL/min/year. That’s a 66% reduction in kidney function loss. One patient in Seattle, diagnosed at Stage 1 after a routine checkup, started taking an SGLT2 inhibitor, cut her sodium intake, and walked 30 minutes daily. Five years later, her eGFR is unchanged. Her uACR dropped from 89 to 22. She’s not on dialysis. She’s not hospitalized. She’s living normally.The Hidden Barriers
Why aren’t more people being screened? Because the system isn’t built for it. Electronic health records rarely remind doctors to order both eGFR and uACR. A 2022 study found that only half of primary care providers consistently order both tests. Many still rely on creatinine alone. And when they do order uACR, they often use random urine samples instead of first-morning voids-which are more accurate. There’s also confusion about race adjustment in eGFR calculations. Some labs still use race-based formulas that underestimate kidney damage in Black patients. New data shows removing race from the formula could increase early detection in Black populations by over 12%. The 2024 KDIGO guidelines are expected to recommend dropping race entirely. And then there’s the cost myth. Screening adds $28-$42 per patient per year. But preventing one case of kidney failure saves over $1,850 in avoided hospitalizations, dialysis, and complications. Medicare spends $120 billion a year on kidney disease. Early detection could cut that by $27 billion annually.What’s Changing Now
The tide is turning. In 2023, the FDA cleared the first AI-powered tool-NephroSight by Renalytix-that analyzes 32 clinical factors to predict CKD risk before eGFR drops. It’s already being used in VA hospitals. The Biden administration’s 2023 Executive Order on Kidney Health includes $150 million to implement dual-testing in Federally Qualified Health Centers by 2026. That’s 1.2 million more people who could be diagnosed early. Point-of-care uACR devices are coming. By 2025, you may be able to get your urine protein result in 10 minutes during a regular doctor visit-no lab needed. And patient education is working. Clinics that use visual charts to show CKD stages (instead of just numbers) see 28% better patient understanding and adherence to treatment.
What You Can Do Today
If you’re at risk:- Ask your doctor for both an eGFR and a uACR test-not just creatinine.
- If your eGFR is between 60 and 89, and you have diabetes or high blood pressure, insist on the uACR test.
- Keep your blood pressure under 130/80.
- Reduce salt. Avoid NSAIDs like ibuprofen unless absolutely necessary.
- Don’t wait for symptoms. By then, it’s often too late.
Frequently Asked Questions
Can chronic kidney disease be reversed?
Early-stage CKD (Stages 1-2) can often be stabilized or even improved with proper treatment. While damaged kidney tissue doesn’t regenerate, stopping further damage is possible. Many patients with Stage 1 CKD maintain stable kidney function for 10+ years with blood pressure control, medication, and diet changes. Progression to later stages is preventable in 60-70% of cases when caught early.
Is a high creatinine level always a sign of kidney disease?
No. Creatinine levels vary based on muscle mass, age, sex, and diet. A young, muscular man may have a creatinine level of 1.3 and perfectly healthy kidneys. An older woman with low muscle mass may have a creatinine of 1.1 and early kidney damage. That’s why eGFR (which adjusts for these factors) and uACR are needed together. Relying on creatinine alone misses up to 40% of early cases.
Do I need a kidney biopsy if I’m diagnosed with CKD?
Almost never. In 98-99% of cases, CKD is caused by diabetes, high blood pressure, or aging-and the treatment is the same regardless of the exact cause. Biopsies are only done if there’s unusual blood in the urine, rapid decline in kidney function, or if the cause is unclear after other tests. Most people never need one.
Can I still drink alcohol if I have early CKD?
Moderate alcohol consumption-up to one drink per day for women and two for men-is generally safe if your blood pressure and diabetes are controlled. But heavy drinking raises blood pressure, dehydrates you, and can worsen kidney damage. Avoid binge drinking and never mix alcohol with NSAIDs like ibuprofen.
Why do some doctors only check creatinine?
Many doctors were trained using older guidelines that focused on creatinine. Some still believe it’s sufficient. Others don’t have time to order two tests or their electronic records don’t prompt them. But current standards require both eGFR and uACR. If your doctor only orders one, ask why-and request the other.
Are there any natural remedies that help CKD?
There’s no proven herbal supplement or detox that reverses kidney damage. Some herbs (like licorice root or aristolochic acid) can actually harm the kidneys. The only proven interventions are blood pressure control, SGLT2 inhibitors, low-sodium diet, and avoiding nephrotoxic drugs. Be wary of products claiming to "cleanse" or "repair" kidneys-they’re not backed by science.




They're testing us. They know we don't check our kidneys. They want us to fail so they can sell us dialysis machines. I saw a video where the lab techs laugh when they see your uACR results. They're all in on it.
This is so important... I just had my first uACR test last month after my doctor finally listened. I'm Stage 2, but my eGFR was fine. I'm on an SGLT2 now, and honestly? I feel better than I have in years. 🌱💧
Of course they don't test you properly. The pharmaceutical industry owns every lab. They profit more from dialysis than prevention. Your 'simple diet changes'? They don't pay enough. You're being manipulated into thinking you're in control.
You know what's funny? The article says 'don't wait for symptoms'-but if you're over 60 and have high blood pressure, your doctor probably already knows you're at risk. The real issue is that most people don't follow up. It's not the system's fault-it's yours.
I'm a nurse. I've seen this too many times. People come in with Stage 4 CKD, and they say 'I didn't know.' No, you didn't care. You drank your soda, took your ibuprofen like candy, and ignored every warning. Now you're mad at the system? Wake up.
If you're diabetic or hypertensive, get both tests. Period. I've helped over 30 patients avoid dialysis just by catching it early. The meds work. The diet works. It's not magic-it's medicine. And it's free with most insurance. Stop waiting for the sky to fall.
i just got my results back and my uacr was 42... i was terrified but my dr said its stage 2 and i can turn it around. i started walking every day and cut out the soda. its scary but i feel like i have power now. thanks for sharing this
The data presented is statistically sound, yet the underlying assumption-that primary care providers are negligent-is a fallacy. The system is under-resourced, not malicious. Furthermore, the race-adjusted eGFR debate is not about bias; it is about physiological variance. To discard it without robust longitudinal validation is premature.
This is one of the clearest, most helpful posts I've read in a long time. Thank you for laying it out so plainly. I'm sharing this with my dad-he's 68 and has diabetes. He's been ignoring his bloodwork for years. Maybe this will finally get through.
You think this is about health? No. This is about control. The government wants you dependent on meds and tests. They don't want you healing naturally. That's why they ban herbs and push expensive pills. I cured my CKD with turmeric and lemon water. No labs needed. They hate that.
I'm a nephrologist. I see this every day. The biggest barrier isn't cost or ignorance-it's time. A good visit with a diabetic patient takes 20 minutes. Most doctors get 10. They order creatinine because it's fast. They don't have the bandwidth to explain uACR. But if you ask for it? They'll do it. Just ask.
You say early detection saves lives. But what if the diagnosis itself kills you? Anxiety, depression, financial ruin from unnecessary meds... isn't that a form of harm? Maybe we should stop pathologizing normal aging. Not every decline is a disease. Maybe the kidneys are just tired.
They say 'don't wait for symptoms'-but guess what? I had swelling, fatigue, and foamy urine. Went to the doctor. They said 'it's just water retention.' Two years later, I was on dialysis. They didn't test me. Not once. This isn't prevention-it's a lie sold by Big Pharma and their lab partners.
I'm a 52-year-old mom with type 2. I got both tests last year after reading this. My uACR was 68. I started walking, cut out processed food, and took my SGLT2. My eGFR is stable. My kids say I'm 'the healthiest mom ever.' It's not perfect. But it's mine. And I'm still here.