When your heart arteries are clogged, two main options exist to restore blood flow: PCI and CABG. Both work, but they’re not the same. One is a quick catheter procedure. The other is open-heart surgery. Choosing between them isn’t about which is better overall-it’s about which is better for you.
What PCI Actually Does
PCI stands for Percutaneous Coronary Intervention. It’s often called angioplasty with stenting. A thin tube (catheter) is threaded from your wrist or groin up to your heart. A tiny balloon is inflated at the blockage to open it. Then, a metal mesh tube called a stent is left behind to keep the artery open. Most stents today are drug-eluting, meaning they slowly release medicine to prevent scar tissue from clogging the artery again.
This isn’t surgery. No incision. No opening your chest. Most people go home the same day or the next. Recovery is fast. Many are back to light activities in a few days. You might feel sore at the access site, but that’s usually it.
PCI works great for single or simple blockages. It’s the go-to for heart attacks-quick, effective, lifesaving. But for complex disease? It has limits. Studies show that if you have multiple blockages, especially in the main left artery or with diabetes, PCI has higher chances of needing another procedure later.
What CABG Actually Does
CABG means Coronary Artery Bypass Grafting. It’s open-heart surgery. Surgeons take a healthy blood vessel from your leg, arm, or chest and use it to create a detour around the blocked artery. Think of it like building a new road around a collapsed bridge.
The most common graft is the left internal mammary artery (LIMA) connected to the left anterior descending (LAD) artery-the main artery feeding the front of your heart. This graft lasts decades. Arterial grafts have an 85-90% chance of staying open after 10 years. Vein grafts (from the leg) are less durable, with about 60-70% patency after 10 years.
CABG takes longer. The surgery lasts 3 to 6 hours. You’ll be in the hospital 5 to 7 days. Full recovery? 6 to 8 weeks. You’ll have a long scar down your chest. Your sternum is wired back together. It hurts. A lot-at first. About 45% of patients still feel sternal pain at 3 months. But by year one, most say it’s gone.
Here’s the catch: CABG doesn’t just fix one blockage. It can bypass multiple arteries at once. That’s why, for complex disease, it often outperforms PCI in the long run.
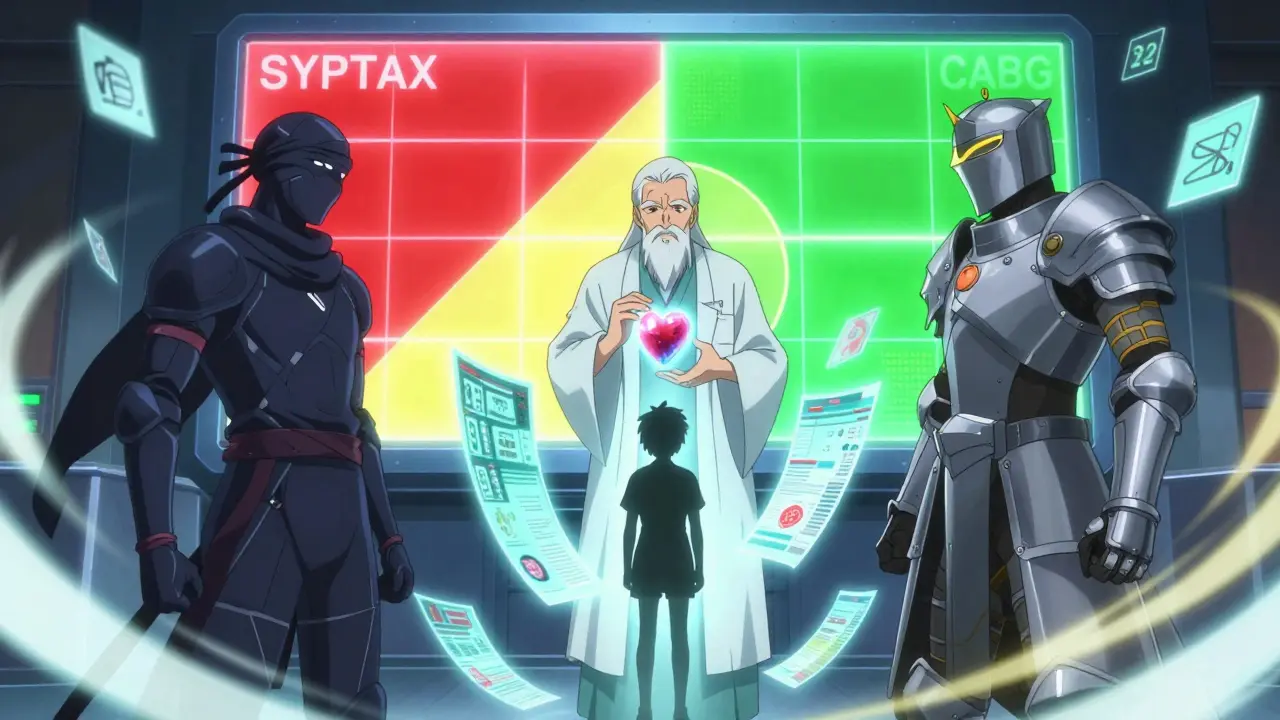
How Doctors Decide: The SYNTAX Score
Doctors don’t pick PCI or CABG based on gut feeling. They use tools. The most important one? The SYNTAX Score. It’s a number based on your angiogram-the X-ray images of your heart arteries.
The score measures how complex your blockages are: number of blockages, location, how much they narrow the artery, whether they’re calcified or branched.
- Score under 22: PCI is usually preferred. Simple disease. Low risk of needing another procedure.
- Score 22 to 32: It’s a gray zone. Heart team discussion is required. Your diabetes, age, and kidney function matter here.
- Score over 32: CABG is strongly recommended. Complex disease. PCI has too high a chance of failure or repeat procedures.
A 2019 meta-analysis of 11,518 patients showed CABG reduced the need for repeat procedures by more than half compared to PCI. That’s huge. If you hate the idea of going back for another stent, CABG gives you more lasting peace.

Who Benefits Most from CABG?
Not everyone needs surgery. But some people have a clear advantage with CABG:
- Diabetics with multivessel disease: The FREEDOM trial found that after 5 years, 16.4% of diabetics who got PCI died. Only 10% of those who had CABG died. That’s a 6.4% absolute survival benefit. For diabetics, CABG isn’t just better-it’s often life-saving.
- Left main disease: This is the main artery feeding most of your heart. Blockage here is dangerous. The EXCEL trial showed PCI and CABG were similar at 3 years. But by 5 years, CABG had fewer heart attacks and repeat procedures. The benefit grows over time.
- People with poor heart function: If your left ventricle is weak (ejection fraction under 40%), CABG improves survival more than PCI.
These aren’t opinions. These are outcomes from large, randomized trials. They’re why guidelines now say CABG is the preferred option for diabetics with multivessel disease.
Why PCI Still Wins for Some
CABG isn’t for everyone. PCI has real advantages:
- Faster recovery: You’re back to work in days, not weeks. One patient on Reddit said, “Back to work in 3 days.”
- Lower stroke risk: At 30 days, stroke risk is about 0.6% with PCI and 1.2% with CABG. That’s half the risk.
- Lower immediate risk: For someone 80 with kidney failure or lung disease, the risks of open surgery might be too high. PCI is safer in high-risk patients.
PCI is also better for people with one or two blockages who aren’t diabetic and have good heart function. If you’re young, active, and have simple disease, PCI is a smart choice.
The Heart Team Matters
Guidelines say the decision should be made by a heart team-not one doctor alone. That means an interventional cardiologist and a cardiac surgeon sit down together, review your scans, and talk to you.
Why? Because each sees the problem differently. The cardiologist thinks: “Can I fix this with a stent?” The surgeon thinks: “Can I build a lasting bypass?”
High-volume centers-those doing over 400 PCIs or 200 CABGs a year-have better outcomes. Mortality for CABG drops from 3.2% in low-volume hospitals to 1.8% in high-volume ones. That’s a 40% difference.
If your hospital doesn’t have a heart team, ask for a referral. This isn’t a decision to make alone.
Quality of Life: Short Term vs Long Term
PCI wins in the short term. At 30 days, 78% of PCI patients feel like normal daily activities. Only 52% of CABG patients do. It’s a big difference.
But at one year? CABG wins. The ROSETTA trial found CABG patients had significantly better angina relief. 92% of CABG patients said they had no chest pain. Only 85% of PCI patients did.
Long-term, CABG patients report better quality of life. They’re more likely to be free of angina. Less likely to need another procedure. Less likely to have a heart attack.
PCI patients often say: “I felt great for a year. Then the chest pain came back. I needed another stent.” That’s common. About 15-20% of PCI patients need a second procedure within 5 years.
What’s Changing Now?
Technology keeps evolving. New stents are thinner, safer, and more effective. Arterial grafts in CABG are now being used more often-not just one, but two or even three. Early data shows 10-year survival jumps from 74% to 82% with multiple arterial grafts.
Robotic-assisted CABG is becoming more common. It’s less invasive, smaller incisions, faster recovery. Still not mainstream, but growing.
And there’s talk of hybrid procedures: a small bypass for the LAD, plus stents for other arteries. This might become the gold standard in 5 to 7 years.
Final Thoughts: No One-Size-Fits-All
PCI is fast. CABG lasts longer. Neither is perfect. The right choice depends on:
- Your SYNTAX score
- Whether you have diabetes
- How many arteries are blocked
- If the left main artery is involved
- Your age and other health problems
- Your recovery goals
If you’re diabetic with multiple blockages? CABG is the better choice. If you’re healthy, have one blockage, and want to get back to work fast? PCI makes sense.
Don’t let fear of surgery push you toward stents if you need a bypass. Don’t let the idea of open-heart surgery scare you if it’s the right choice. Talk to your heart team. Ask for your SYNTAX score. Understand the long-term trade-offs. Your heart will thank you.
Is PCI safer than CABG?
PCI has lower immediate risks, especially for stroke and major bleeding. But CABG has lower long-term risks of heart attack and repeat procedures. For high-risk patients (elderly, kidney disease), PCI is safer short-term. For complex disease, CABG is safer long-term.
Can I choose PCI if I’m diabetic?
Yes, but it’s not the best choice. Diabetics with multivessel disease have a 76% higher risk of death after PCI compared to CABG, based on the FREEDOM trial. CABG is the recommended option for diabetics with complex disease.
How long do stents last?
Modern drug-eluting stents last 5-10 years in most patients. But about 5-10% of patients need another procedure within 5 years. If the artery re-narrows, you may need another stent or even CABG later.
Does CABG cure heart disease?
No. CABG improves blood flow, reduces symptoms, and lowers risk of heart attack. But it doesn’t stop plaque from building up elsewhere. Lifestyle changes-diet, exercise, quitting smoking, taking meds-are still essential.
What’s the recovery time for CABG?
Hospital stay: 5-7 days. Full recovery: 6-8 weeks. You can drive in 4-6 weeks. Return to work: 6-12 weeks, depending on your job. Most people feel like themselves again by 6 months.




I had PCI last year after a minor heart scare. Back to work in 3 days. No scar, no pain, just a tiny bruise. People act like surgery is the only real fix but sometimes the easy way is the smart way. My cardiologist said I was a perfect candidate. Don’t let fear scare you into open-heart if you don’t need it.
Honestly? I think CABG is overhyped. I’ve seen three people go through it. Two of them still have chest pain. One guy’s sternal wire started poking through his skin two years later. Meanwhile, my buddy got a stent and hasn’t had a single issue. Maybe it’s just luck but… I’m not convinced surgery is always better.
The SYNTAX score is a joke. I work in hospital admin and I’ve seen docs pick PCI for patients with scores over 32 because their insurance won’t cover CABG. And don’t get me started on how ‘heart teams’ are just two docs arguing in a room while the patient signs a waiver. 🤡
There’s a deeper truth here: medicine isn’t about picking the ‘best’ option-it’s about picking the least bad one for your life. If you’re 52 and run marathons, CABG might mean a year off. If you’re 70 and just want to play with your grandkids? PCI might be the gift of time. Neither is perfect. Both are tools.
It is imperative to emphasize that the decision-making process must be grounded in evidence-based guidelines and multidisciplinary evaluation. The SYNTAX score, while not infallible, remains one of the most validated tools for risk stratification. Patient autonomy must be balanced with clinical expertise.
Let me tell you what no one talks about: the stent you get today might be obsolete in 5 years. New ones are thinner, coated with better drugs, last longer. Meanwhile, CABG grafts? We’ve been using the same leg vein grafts since the 80s. Yeah, LIMA’s great-but most hospitals still use veins because it’s easier. The system’s stuck in the past.
You got this. I was scared of CABG too. But my surgeon said if I didn’t do it, I’d be back in 2 years with another heart attack. Now I’m 3 years out, no meds except aspirin, and I hike every weekend. It hurts at first but it’s worth it. You’re stronger than you think. 💪
Oh wow. So we’re just gonna ignore that 80% of stents fail within 10 years? And that CABG survival rates are 2x better in diabetics? This post is basically Big Pharma’s ad. You think they want you to know that a $30k stent needs replacing? Nah. They want you to keep coming back for more. 🤑
This whole thing is a scam. The heart team? They’re paid by the hospital. The SYNTAX score? Made by a company that sells angiography machines. And don’t even get me started on how stents are pushed because they’re profitable. They don’t care if you live 10 years or 5. They just want your insurance to pay.
In India we don’t even have access to proper CABG in most places. Stents are everywhere because they’re cheaper. But you know what? We still have better survival rates than the US because we eat real food, walk everywhere, and don’t sit on couches all day. This whole Western medical system is broken.
I appreciate the thorough breakdown. The data presented here aligns with current ACC/AHA guidelines. The emphasis on heart team evaluation is particularly crucial, as it mitigates physician bias and improves outcomes. Well-researched piece.
I had CABG 4 years ago. 3 arterial grafts. Still feel like a new man. But here’s the thing: my wife cried for 3 weeks. The recovery wasn’t just hard for me-it broke her. If you’re thinking about surgery? Talk to your partner first. This isn’t just about your heart. It’s about your whole life.
i had pci last year. felt great. 6 months later i got chest pain again. did another stent. now im on my third. my doc says 'its normal' but i feel like i’m just getting patched up like a tire. maybe i should’ve gone for the surgery. idk anymore.
I’m a nurse who’s seen both. PCI is like a Band-Aid. CABG is like a full remodel. You want quick? Go PCI. You want peace? Go CABG. I had my dad do CABG. He’s 80 now, still gardening. No meds. No pain. Just quiet. Don’t let fear make you choose the easy path if the hard one is the right one.
I’ve been reading all these comments and I just want to say this: the real hero here isn’t the stent or the graft. It’s the person who asked for a second opinion. Who insisted on the SYNTAX score. Who didn’t just sign the form. You have to be your own advocate. That’s what saved my life. Not the tech. Not the doctor. Me.