After losing a limb, some people still feel pain in the part that’s no longer there. It’s not in their head. It’s not imaginary. It’s real - and it’s called phantom limb pain. Around 60% to 85% of amputees in the U.S. deal with it. That’s more than half of everyone who’s had an amputation. The pain can feel like burning, cramping, or electric shocks in a foot or hand that’s gone. For many, it starts within weeks after surgery. If it lasts longer than six months, it rarely goes away on its own. That’s why treatment isn’t optional - it’s necessary.
Why Phantom Limb Pain Happens
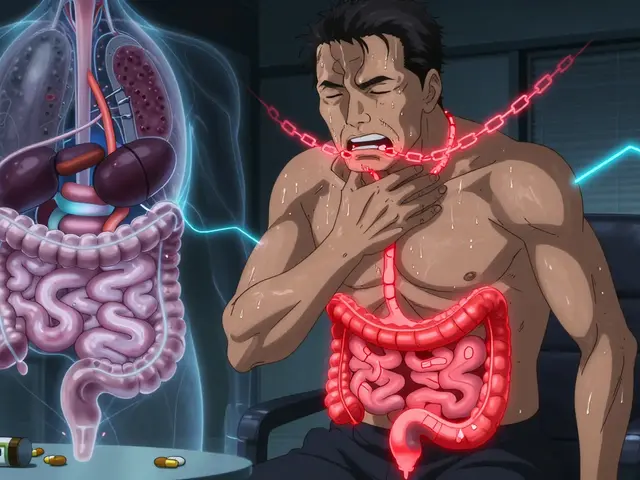
For decades, doctors thought phantom limb pain was psychological. Then came brain scans. MRI and PET scans showed clear activity in the parts of the brain that used to control the missing limb. When a person feels pain in their phantom hand, the brain region that once handled signals from that hand lights up. That’s not stress. That’s neurology.
The body’s nervous system doesn’t just shut off after amputation. Damaged nerves at the stump send mixed signals. The spinal cord and brain try to make sense of them. Over time, the brain rewires itself - a process called cortical remapping. Areas that once received input from the amputated limb start responding to nearby body parts. Touch your face, and suddenly your phantom leg tingles. That’s why triggers like pressure on the stump, stress, cold weather, or even an ill-fitting prosthesis can make the pain worse.
Medications: What Works and What Doesn’t
Most people start with medication. It’s the most common first step. But not all drugs work the same for everyone. The goal isn’t to eliminate pain completely - it’s to reduce it enough to live better.
- Tricyclic antidepressants like amitriptyline (10-75 mg daily) and nortriptyline are the most prescribed. They don’t treat depression here - they calm overactive nerves. About 45% of users report moderate relief, but 60% say they feel drowsy or dry-mouthed.
- Anticonvulsants like gabapentin (300-3600 mg daily) and pregabalin (75-600 mg daily) are next in line. A Reddit survey of 147 amputees found 72% found gabapentin helpful, but 58% quit because of dizziness or weight gain.
- NSAIDs like ibuprofen or naproxen help some people at first. But for 80% of users, the effect fades after 3-6 months. They’re not a long-term solution.
- Ketamine (given IV at 0.1-0.5 mg/kg) is used for severe cases that don’t respond to anything else. It works by blocking NMDA receptors, which are involved in pain memory. But it’s not for everyone - it can cause hallucinations or dizziness.
- Opioids like oxycodone or morphine are still used, but they’re controversial. The American Pain Society warns against daily doses above 50 morphine milligram equivalents (MME). Long-term use leads to dependence in about 35% of users, according to PainManagement.org.
- Botulinum toxin (Botox) injections into the stump can help if neuromas (nerve bundles) are causing pain. One 2023 case study showed pain dropping from 8/10 to 3/10 for 12 weeks.
There’s no magic pill. Most patients try 2-3 medications before finding one that works. Dosing starts low. It takes weeks to adjust. Side effects are common. That’s why many people look beyond pills.
Mirror Therapy: Seeing Is Believing
Imagine sitting in front of a mirror. You place your intact limb on one side. The mirror reflects it, making it look like your missing limb is still there. Then you move it - slowly, gently. Wiggle your fingers. Flex your ankle. Your brain sees movement where there should be none. And over time, that visual feedback helps retrain the brain.
This is mirror therapy. It was pioneered by neuroscientist V.S. Ramachandran in the 1990s. His work showed that when the brain sees movement in the phantom limb, it starts to unlearn the pain signals. No drugs. No needles. Just a mirror and 15-30 minutes a day.
It’s not magic. It takes discipline. A 2021 study in the Physical Therapy Journal found that 40% of patients quit mirror therapy within eight weeks. Why? It feels silly at first. It’s hard to stay consistent. But those who stick with it? Many report a 30-50% drop in pain intensity. Some say the pain disappears for hours after a session.
Modern versions now use virtual reality headsets. Instead of a mirror, you see a digital version of your missing limb moving in sync with your good limb. Early trials suggest this boosts adherence - maybe because it’s more engaging. By 2027, experts predict VR-based mirror therapy could help 85% of users stick with it, up from today’s 60%.

Other Non-Medication Options
Medication isn’t the only path. Several other tools are used in clinics across the U.S.:
- TENS (Transcutaneous Electrical Nerve Stimulation): Electrodes on the stump deliver mild pulses. It’s FDA-cleared. About 30-50% of users get relief. It’s cheap, portable, and non-invasive.
- Spinal cord stimulation: A small device implanted near the spine sends pulses to block pain signals. In 2024, the FDA approved a new closed-loop system called Evoke from Saluda Medical. It adjusts automatically. In trials, it cut pain by 65% on average.
- Biofeedback: Sensors show you your body’s stress signals - heart rate, muscle tension. You learn to calm them. Studies show 25-40% effectiveness. It works best with trained therapists.
- Targeted muscle reinnervation: Surgeons reroute nerves from the amputated limb to nearby muscles. When the patient thinks about moving the phantom limb, the muscle contracts. Combined with osseointegration (a metal implant in the bone), this approach cut pain by 70% in a 2024 Journal of Neurosurgery study.
These aren’t replacements for medication - they’re partners. The best outcomes come from combining them.
What Experts Say
Doctors don’t treat phantom limb pain with one tool. They use a team approach. A 2025 Fast Fact from the Palliative Care Network of Wisconsin says: “Multiple mechanisms are likely responsible.” That means you need multiple treatments.
One big myth? That giving strong pain meds during surgery prevents phantom pain later. Research now says that’s not true. Epidural anesthesia doesn’t stop it.
Another myth? That it’s all in your head. Brain scans prove otherwise. The pain is real. The brain is misfiring. The goal isn’t to ignore it - it’s to rewire it.
Early action matters. If you’re in pain six months after amputation, don’t wait. The chances of it going away on its own? Slim to none.

Real People, Real Results
Some stories stand out:
- A 52-year-old man in Ohio tried four medications. None worked. He started mirror therapy with a $20 mirror box. After six weeks, his pain dropped from 9/10 to 4/10. He now does it daily while watching TV.
- A woman in Texas had severe phantom cramping. Her doctor gave her botulinum toxin injections. The pain dropped to 3/10 and stayed there for 12 weeks. She had to repeat it every 4 months.
- A veteran in Seattle got spinal cord stimulation. He went from being unable to sleep to riding his bike again. His pain score went from 8/10 to 2/10.
But not everyone wins. Some try everything - meds, TENS, mirror therapy - and still struggle. That’s why research keeps going. New drugs targeting NMDA receptors are in Phase II trials. They promise 50% pain reduction with fewer side effects than ketamine.
Where to Start
If you or someone you know has phantom limb pain:
- See a pain specialist. Not just an amputee clinic - a pain management team.
- Start with low-dose amitriptyline or gabapentin. Give it 4-6 weeks.
- Try mirror therapy. Buy a mirror box ($30-$80 online). Do 15 minutes a day. No need to be perfect.
- Ask about TENS. It’s covered by most insurance.
- If pain stays above 6/10 after 3 months, ask about spinal cord stimulation or botulinum toxin.
- Join a support group. The Amputee Coalition has 12,000+ members. Talking to others who get it helps more than you think.
There’s no one-size-fits-all fix. But there’s hope. And there are real tools - backed by science, tested in clinics, and used by real people every day.
Is phantom limb pain psychological?
No. While it was once thought to be psychological, brain imaging studies show clear activity in areas of the brain that once controlled the missing limb. This confirms phantom limb pain is a neurological condition, not a mental one.
Can mirror therapy cure phantom limb pain?
Mirror therapy doesn’t cure it, but it can significantly reduce pain for many people. Studies show 30-50% of users get meaningful relief. It works by helping the brain relearn how to process movement without triggering pain signals. Consistency matters - most people need to do it daily for weeks to see results.
Which medications are most effective for phantom limb pain?
Tricyclic antidepressants like amitriptyline and anticonvulsants like gabapentin are the most commonly prescribed and effective. They target nerve pain directly. About 45-72% of users report improvement, though side effects like drowsiness or dizziness are common. Ketamine and opioids are used for severe cases but carry higher risks.
Why does phantom limb pain last so long?
The brain rewires itself after amputation. Areas that once received signals from the missing limb begin responding to nearby body parts. This process, called cortical remapping, can create false pain signals. If pain lasts more than six months, the brain has essentially learned the pain pattern. Without intervention, it rarely fades on its own.
Are there new treatments on the horizon?
Yes. In early 2024, the FDA approved a new spinal cord stimulation system called Evoke that adjusts automatically to pain signals. Clinical trials showed 65% average pain reduction. Researchers are also testing new NMDA receptor drugs that mimic ketamine’s effects without side effects. Virtual reality mirror therapy is expected to improve adherence rates by 2027, making treatment more effective.
Phantom limb pain is complex, but it’s not untreatable. The key is starting early, staying consistent, and combining tools - medication, movement, and technology. You don’t have to live with pain that shouldn’t exist. Help is out there.