Why Generic Drug Coverage Matters More Than You Think
When you switch health plans, most people focus on monthly premiums, doctor networks, or hospital coverage. But one of the biggest surprises-and most expensive mistakes-comes from generic drug coverage. If you take even one regular medication, skipping this step can cost you hundreds or even thousands of dollars a year.
Here’s the reality: 90% of all prescriptions filled in the U.S. are generics. They work just like brand-name drugs but cost a fraction of the price. Insurance companies know this, so they structure their plans to push you toward generics. But not all plans treat them the same. Some charge $3 a month. Others make you pay the full deductible before you get any coverage. That difference isn’t minor-it’s life-changing for people managing diabetes, high blood pressure, or thyroid conditions.
How Formularies Work: The Hidden Rules Behind Your Copay
Your plan’s formulary is the official list of drugs it covers, divided into tiers. Each tier has a different price. The key to saving money? Knowing which tier your generic is in-and how that tier works with your deductible.
Most plans use 3 to 5 tiers:
- Tier 1: Preferred generics. Usually $3-$20 for a 30-day supply. This is where you want your meds to be.
- Tier 2: Non-preferred generics or brand-name drugs with generic alternatives. Often $30-$50.
- Tier 3: Preferred brand-name drugs. $50-$100.
- Tier 4 and 5: Non-preferred brands and specialty drugs. These can cost hundreds.
But here’s what no one tells you: not all generics are created equal. Your plan might cover metformin (a common diabetes drug), but only if it’s made by Manufacturer A. Switch to Manufacturer B? Suddenly, it’s a Tier 2 drug. Same active ingredient. Same effectiveness. Different price. That’s why you can’t just look up the drug name-you need the exact brand and dosage.
Marketplace Plans vs. Medicare vs. Employer Plans: What’s Different?
Not all health plans follow the same rules. The type of plan you’re switching to changes how your generics are covered.
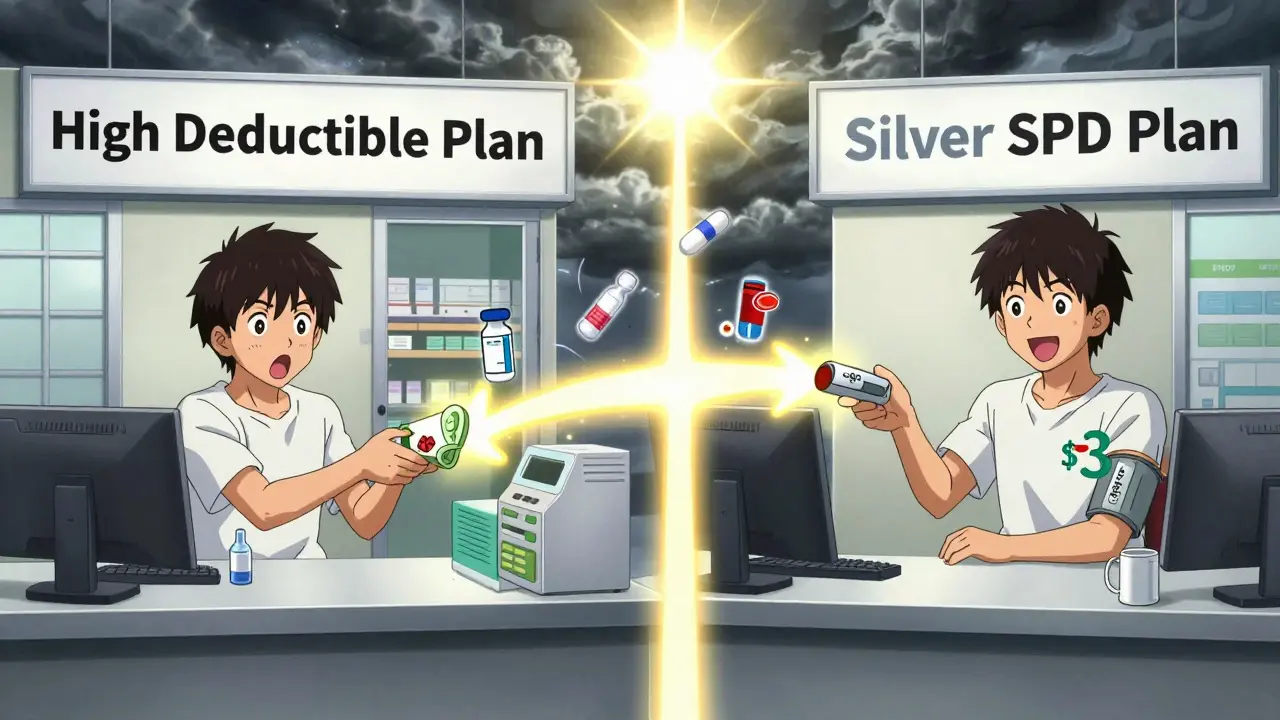
Marketplace plans (Healthcare.gov) must follow federal rules. Silver-level plans with Standardized Plan Design (SPD) waive the deductible for Tier 1 generics. That means you pay just $20 or less per prescription-no matter how much you’ve spent on medical care. These plans are the best deal if you take regular generics. In 2025, 32 states offer expanded SPD options with $10 copays.
High-deductible health plans (HDHPs) are trickier. They combine your medical and prescription deductibles. So if your deductible is $3,000, you pay full price for every pill until you hit that number. That’s a disaster if you need daily meds. Some HDHPs have separate prescription deductibles, but most don’t. Always check.
Medicare Part D has its own system. The base deductible in 2025 is $505, but many plans waive it for Tier 1 generics. Copays range from $0 to $10. Medicare Advantage plans with drug coverage (MA-PDs) often have lower out-of-pocket costs than standalone Part D plans-by about 18% on average. But watch out: formularies change every year. A drug that was Tier 1 last year could move to Tier 2.
Employer plans vary wildly. Some companies offer $5 copays for generics. Others make you pay full price until you meet a $1,500 deductible. If you’re switching jobs, don’t assume your current meds will be covered the same way.
State Rules Can Make or Break Your Savings
Where you live matters. States have their own rules that override federal guidelines.
- In New York, generic copays are often $0 or $7 before any deductible.
- In California, you pay a $85 outpatient drug deductible first, then 20% coinsurance (capped at $250 per year).
- In Washington D.C., there’s a separate $350 drug deductible with a $150 cap on specialty drugs.
These differences aren’t theoretical. A person in New York taking three generics might pay $0 a month. In California, they could pay $40 a month-$480 a year. That’s a $480 gap just from geography.
How to Check Your Medications Before You Switch
Don’t guess. Don’t rely on a sales rep. Do this four-step check before you sign up for a new plan:
- Get the full formulary-not just the summary. Look for the PDF or searchable list on the insurer’s website.
- Search for every drug you take, including dosage and manufacturer. Type in “metformin 500mg, Teva” not just “metformin.”
- Check your pharmacy network. Some plans charge 3-4 times more if you use a non-preferred pharmacy. Use CVS, Walgreens, or your local pharmacy? Confirm they’re in-network.
- Calculate your annual cost. Multiply your monthly copay by 12. Add any deductible you must meet. Include mail-order discounts if you use them.
People who do this reduce unexpected drug costs by 73%, according to CMS data. Those who skip it? They’re the ones calling their insurer in March, confused why their $5 pill suddenly costs $45.
Tools That Actually Work
You don’t need to dig through 50 pages of fine print. Use these free tools:
- Medicare Plan Finder (medicare.gov/plan-compare): Best for seniors. Lets you enter all your drugs and compares plans side by side.
- Healthcare.gov Plan Selector: Filters plans by drug coverage. Shows you which ones waive deductibles for generics.
- eHealthInsurance’s Prescription Calculator: Processes over 1.7 million queries a month. Fast, simple, accurate.
- Insurer-specific tools: Blue Cross, UnitedHealthcare, and Humana all have their own formulary searchers. These are usually the most accurate-96% accuracy vs. 78% on third-party sites.
Use at least two tools. Cross-check. If one says your drug is Tier 1 and another says Tier 2, call the insurer. Don’t trust the website alone.
What No One Tells You About Generic Switches
Manufacturers change. And when they do, your plan might stop covering your version.
Example: You take generic levothyroxine made by Mylan. Your plan covers it at $3. In January, your insurer switches to a different manufacturer-Teva. Mylan’s version is no longer on the formulary. Now your drug is Tier 2: $35. You don’t get a notice. You don’t find out until you refill your prescription.
This happens to 15% of Medicare beneficiaries every year. The American Pharmacists Association found that 68% of people switching plans don’t check if their specific generic version is still covered. They assume “generic” means “same price.” It doesn’t.

What’s Changing in 2025
Things are shifting fast. Here’s what to watch:
- Medicare Part D is adding a new tier: Tier 1+ for non-preferred generics. This could raise costs for people on older generic versions.
- $35 insulin cap is now permanent. If you take insulin, you pay no more than $35 a month-no matter your plan.
- $2,000 out-of-pocket cap for Medicare Part D starts in 2025. Once you hit that, your drugs are free for the rest of the year.
- AI tools like Medicare Plan Scout (launched in 2023) are now helping users avoid errors. In pilot tests, they cut enrollment mistakes by 44%.
These changes make it easier to predict costs-but only if you stay informed.
Real People, Real Savings
One woman in Seattle switched from a high-deductible plan to a Silver SPD plan. She takes three generics: metformin, lisinopril, and levothyroxine. Her old plan had a $3,000 deductible. She paid $1,800 a year just for pills. Her new plan? $3 copays. Total annual cost: $108. She saved $1,692.
A retired veteran in Florida used Medicare Plan Finder and found a plan that covered his generic blood pressure med at $0. His previous plan charged $12. That’s $144 saved a year-money he now uses for groceries.
These aren’t outliers. They’re people who took 30 minutes to check their formulary. That’s all it took.
Final Checklist Before You Switch
- ☐ I have a full list of all my medications, including dosage and manufacturer.
- ☐ I checked the new plan’s formulary for each drug-not just the summary.
- ☐ I confirmed my pharmacy is in-network.
- ☐ I calculated my annual cost: copays + deductible + mail-order savings.
- ☐ I used at least two tools to verify my findings.
- ☐ I called the insurer to confirm one drug I’m unsure about.
If you check all these boxes, you’re ahead of 80% of people switching plans. And you won’t be the one shocked by your pharmacy bill next month.
What if my generic drug isn’t covered at all in the new plan?
If your drug isn’t on the formulary, you have a few options. First, ask your doctor if there’s a similar generic that is covered. If not, you can request a formulary exception from your insurer. This requires a letter from your doctor explaining why you need that specific drug. Approval rates are high if you’ve been on it for over a year. If denied, you can appeal or pay out-of-pocket for a few months until open enrollment next year.
Do mail-order pharmacies offer better prices for generics?
Yes, often. Most plans charge less for a 90-day supply through mail-order than three 30-day retail fills. For example, a $15 retail copay becomes $45 for three months. Mail-order might be $30 for the same 90 days. That’s $15 saved. Some plans even waive the deductible for mail-order generics. Always compare the math before you choose.
Can I switch plans mid-year if my drug coverage changes?
Generally, no. You can only switch during open enrollment (November-December for marketplace plans, October-December for Medicare). But if your drug is removed from the formulary mid-year, that’s considered a “material change.” You may qualify for a Special Enrollment Period. Contact your insurer or Medicare right away to ask. Don’t wait until you’re out of pills.
Are there limits on how many generics I can get per month?
Some plans limit quantity per fill-for example, only 30 days at a time unless you’re on a maintenance drug. Others cap the number of prescriptions per month. Check your plan’s “quantity limits” section. If you need more than the limit, your doctor can request an override. This is common for people with multiple chronic conditions.
Why do two identical generics cost different amounts on the same plan?
Because insurers negotiate prices with manufacturers. One version might be cheaper because the manufacturer gave the insurer a better deal. It’s not about quality-it’s about contracts. Your plan labels the cheaper version as “preferred” (Tier 1) and the other as “non-preferred” (Tier 2). Always check the manufacturer name on your prescription label. If it changes, your cost might jump.
Next Steps: What to Do Today
If you’re thinking about switching plans, don’t wait. Right now, get your current list of medications. Open your insurer’s formulary page. Search each drug. Write down the tier and copay. Then, do the same for any plan you’re considering. Compare the totals. If your annual cost drops by $500 or more, it’s worth switching.
Don’t let a small oversight cost you big. Generic drugs are the cheapest way to treat chronic conditions. But only if your plan lets you use them without a financial penalty. Take 30 minutes today. You’ll thank yourself next January when your pharmacy bill is lower than last year’s.




I swear, I didn't even know generics could have different manufacturers until my insulin bill jumped $80 overnight. Turns out my plan switched from Mylan to Teva and I didn't get a single email. 🤯 Now I check the label like it's a lottery ticket. Don't be me.
This article is painfully accurate but fundamentally flawed. The entire U.S. pharmacy benefit management system is a cartelized nightmare. Why are we even discussing tiered copays when the real issue is PBMs squeezing manufacturers and then gouging patients? You're optimizing the wrong variable. Fix the middlemen, not your formulary.
I really appreciate this guide. It's clear, practical, and well-structured. I've shared it with my mom who's on Medicare. She didn't realize her $12 pill was now $47 because of a manufacturer switch. Thank you for making this less intimidating. (Typo: 'medicare.gov/plan-compare' should be 'medicare.gov/plan-compare'-but you knew that.)
People are literally dying because they can't afford their meds. And you're giving them a checklist? That's not a solution-that's a bandage on a severed artery. The system is broken. Stop telling people to 'check their formulary' and start demanding universal drug pricing. This isn't personal finance-it's a moral failure.
OMG YES. I just switched plans and almost blew it. I thought 'generic' meant 'cheap.' Nope. My levothyroxine went from $3 to $38 because they switched from Teva to Mylan. I called my doctor, they got me an exception, and now I'm back to $5. DO NOT SKIP STEP 2. Seriously. Your life is on that label.
Bro, this is why I love info like this 🙌 I'm from India, and here generics are the norm-but we don't have this tier nonsense. Still, your breakdown is gold. I'm sharing this with my cousin in Texas who's on Medicaid. He'll thank me later 😊
While the article provides a superficially competent overview, it fundamentally misrepresents the structural inequities inherent in pharmaceutical cost allocation. The notion that individual consumer diligence can meaningfully offset systemic market failures is not merely optimistic-it is dangerously naive. One does not solve PBM monopolies by memorizing tier structures.
So let me get this straight. You're telling me I need to become a pharmacist, a lawyer, and a spreadsheet wizard just to buy my blood pressure pills? And this is the 'American healthcare system'? Cool. Cool cool cool. 😌
Great summary. One thing to add: if your drug gets moved to a higher tier mid-year, ask your pharmacist for a 30-day 'transition supply.' Most insurers will give you a one-time grace period. It’s not guaranteed, but it’s worth asking. You’ve got rights.
I spent three hours last week digging through my plan’s formulary PDF-217 pages, tiny font, no search function, and the link on the website was broken. I had to call customer service, get transferred five times, and then the rep said, 'Oh, we just updated it yesterday, so the website is outdated.' So I had to print out the new formulary from the fax machine they emailed me? Yes. I did. I cried. I am now a certified formulary detective. And I still don’t trust any of it. This system is designed to break you. Don’t let it.
How quaint. You think checking formularies is the solution? That’s like telling someone to check the weather before stepping into a hurricane. The entire structure is rigged. Manufacturers pay insurers to favor their versions. Insurers reward PBMs for excluding cheaper alternatives. And we’re supposed to be grateful for a $3 copay? Please. This isn’t healthcare-it’s a corporate game of musical chairs with your life-saving pills. Wake up.