Chronic Obstructive Pulmonary Disorder (COPD) — Practical Guide
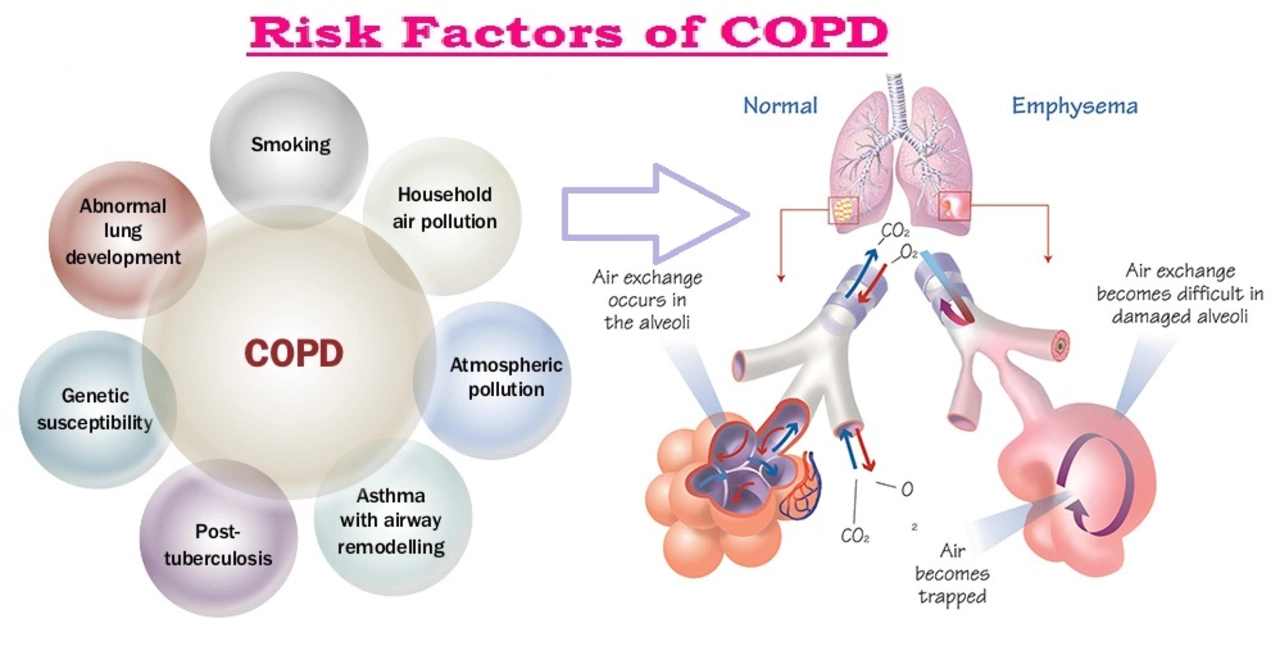
If you or someone you care about has been told they have chronic obstructive pulmonary disorder (COPD), you probably want straightforward advice, not medical jargon. COPD is a long-term lung condition that makes breathing harder over time. Most people notice a cough that won’t go away, shortness of breath when walking or climbing stairs, and more mucus than usual. Smoking is the most common cause, but air pollution, workplace dust, and past lung infections can also play a role.
What to watch for
Early signs are easy to miss. Does walking to the mailbox leave you winded? Do you cough up yellow or green mucus more often? Those are red flags. Flare-ups (exacerbations) bring worse breathlessness, higher cough frequency, fever, or chest tightness. If you ever experience sudden severe breathlessness, blueness around the lips, or confusion, get urgent care.
Diagnosis usually starts with a quick breathing test called spirometry. Doctors may also order chest X-rays, CT scans, or blood tests to rule out infections or heart problems. Pulmonary edema (fluid in the lungs) can feel like severe breathlessness; read our article "Understanding Oedema: Peripheral, Cerebral, And Pulmonary Swelling Explained" for clear differences and signs to watch for.
Everyday care and treatments
Treatment aims to ease symptoms, slow decline, and prevent flare-ups. Inhaled bronchodilators help open airways and are the backbone of COPD care. Some people also need inhaled corticosteroids or long-acting combinations. Oxygen therapy can help when blood oxygen is low. Pulmonary rehab — a supervised program of exercise and breathing techniques — often improves stamina and quality of life more than you’d expect.
Small changes matter. Quitting smoking is the single best step you can take. Keep vaccinations up to date (flu and pneumococcal shots reduce the risk of severe infections). Learn breathing techniques like pursed-lip breathing for quick relief, and pace daily tasks to avoid getting too breathless. A registered dietitian can help if low appetite or weight loss is an issue.
Medicines that relieve coughing, treat infections, or manage nausea may come up. For example, our guide on "Phenergan: Essential Guide for Safe Use, Benefits, and Side Effects" explains when that drug is useful and cautions about mixing meds. Also, be careful about buying potent medicines online — articles like "Steroids-World.com: Safe Online Steroid Pharmacy, Prices, and Legal Tips" discuss risks of purchasing steroids and other prescription drugs without a proper prescription.
Plan for flare-ups. Keep a short action plan: who to call, which meds to start, and when to visit the ER. Track symptoms in a simple notebook or app so you can spot patterns. If breathing gets worse over a few days despite home treatment, contact your provider.
Want more targeted reads? Check our pieces on pulmonary oedema, natural immune support like "Discover the Power of Umckaloabo for Immune Support," and practical drug guides. If you have questions about specific medicines or need help finding reliable sources, our site is here to guide you through the options and next steps.
The Impact of Chronic Obstructive Pulmonary Disorder on Work and Employment
As a blogger, I've recently been researching the impact of Chronic Obstructive Pulmonary Disorder (COPD) on work and employment. I found that this condition can significantly reduce an individual's ability to remain in the workforce, leading to financial strain and a lowered quality of life. The symptoms of COPD, such as shortness of breath and fatigue, can make it difficult for sufferers to perform their job duties effectively. Employers and coworkers may also lack understanding of the condition, contributing to a challenging work environment for those affected. Overall, it's crucial for both employees and employers to be aware of COPD's impact on work and to accommodate those suffering from this disorder to ensure their well-being and productivity.
- View More
- 10