Gastroesophageal Reflux Disease (GERD): What to Know
Heartburn more than twice a week? That might be GERD. Gastroesophageal reflux disease happens when stomach acid flows back into the esophagus and irritates the lining. It can be occasional or chronic, and it affects people of all ages.
Common signs include a burning feeling in the chest, sour taste in the mouth, regurgitation, burping, and bloating. Some people only get a chronic cough, hoarse voice, throat clearing, or trouble swallowing. Pay attention to patterns — when symptoms follow big meals, spicy food, or lying down, reflux is likely.
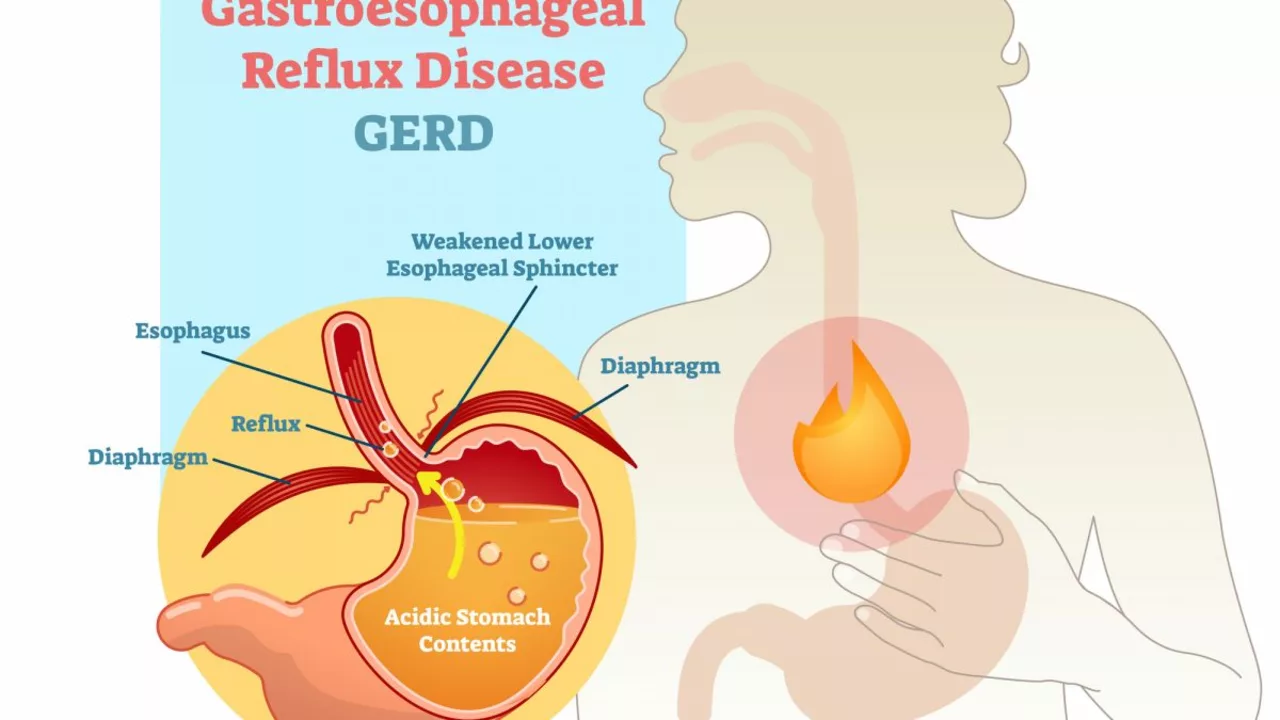
Why does reflux happen? The main problem is the lower esophageal sphincter (LES). If the LES relaxes too often or weakens, acid slips up from the stomach. Other factors raise risk: being overweight, pregnancy, hiatal hernia, smoking, and certain medicines like some painkillers and antidepressants.
Food and habits matter. Common triggers are fatty meals, fried food, chocolate, caffeine, citrus fruits, tomato products, peppermint, alcohol, and spicy dishes. Eating late, large portions, and tight clothing around the waist also make reflux worse. Try to notice which foods hit you hardest and avoid them.
Simple lifestyle moves can cut symptoms fast. Eat smaller meals and stop eating two to three hours before bed. Raise the head of your bed by 6 to 8 inches so gravity helps keep acid down. Drop extra weight if you can, and quit smoking. Swap very spicy or acidic meals for low-acid choices like oatmeal, steamed vegetables, lean protein, and non-citrus fruits.
Over-the-counter options can help too. Antacids give quick relief for mild flare-ups. H2 blockers reduce acid for several hours. Proton pump inhibitors (PPIs) are stronger and used for frequent reflux, but they should be used under a doctor’s guidance. Long-term PPI use has risks, so check with your provider about the right dose and duration.
When to see a doctor? Get urgent help if you have severe chest pain, trouble breathing, vomiting blood, black stools, or weight loss without trying. For ongoing reflux, a doctor may order tests like endoscopy, pH monitoring, or motility studies to check for damage and guide treatment.
Track your symptoms in a simple notebook or app. Note what you eat, when symptoms start, and what helps. That record makes appointments more useful and helps you find real triggers. With a mix of smart habits, diet tweaks, and the right meds, most people can get reflux under control and sleep better at night.
Daily tips that help
Small habits add up. Start meals with water or herbal tea, avoid carbonated drinks, and chew slowly. Wear loose clothes after eating and avoid bending over for a while. If stress makes your symptoms worse, try short breathing exercises or a ten minute walk after meals. If you use OTC pills often, talk to your pharmacist about interactions with other medicines. For pregnancy-related reflux, talk to your doctor about safe antacids and lifestyle steps before taking stronger drugs.
Ask questions and get a plan that fits your life.
Tympanites and Gastroesophageal Reflux Disease (GERD): Understanding the Link
As a blogger, I've recently been researching the link between Tympanites and Gastroesophageal Reflux Disease (GERD). I discovered that both conditions involve the digestive system and can cause discomfort, but they occur in different areas. Tympanites is the excessive presence of gas in the stomach or intestines, while GERD is a chronic disease where stomach acid frequently flows back into the esophagus. It turns out that certain factors, such as diet and stress, can contribute to the development of both conditions. In my research, I've found it crucial to understand the link between these two disorders to better manage their symptoms and improve overall digestive health.
- View More
- 17