Introduction to Tympanites and GERD
As a health-conscious individual, it's essential to understand the various conditions that may affect our digestive system. Today, I'll be discussing Tympanites and Gastroesophageal Reflux Disease (GERD), two common yet often misunderstood conditions. It's crucial to know how they're linked, what causes them, and the possible treatment options available. In this article, we'll explore these topics in detail, aiming to provide a comprehensive understanding of these digestive disorders.
Understanding Tympanites: Causes and Symptoms
Tympanites, also known as abdominal bloating, is a condition characterized by the excessive accumulation of gas in the stomach and intestines. This leads to a feeling of fullness, discomfort, and sometimes pain in the abdominal area. The main causes of tympanites include swallowing air while eating, drinking carbonated beverages, certain food intolerances, and the presence of bacteria in the digestive tract. Some common symptoms associated with tympanites are abdominal pain, cramps, and a visible increase in abdominal size. Additionally, in some cases, sufferers may experience flatulence, belching, and a decreased appetite.
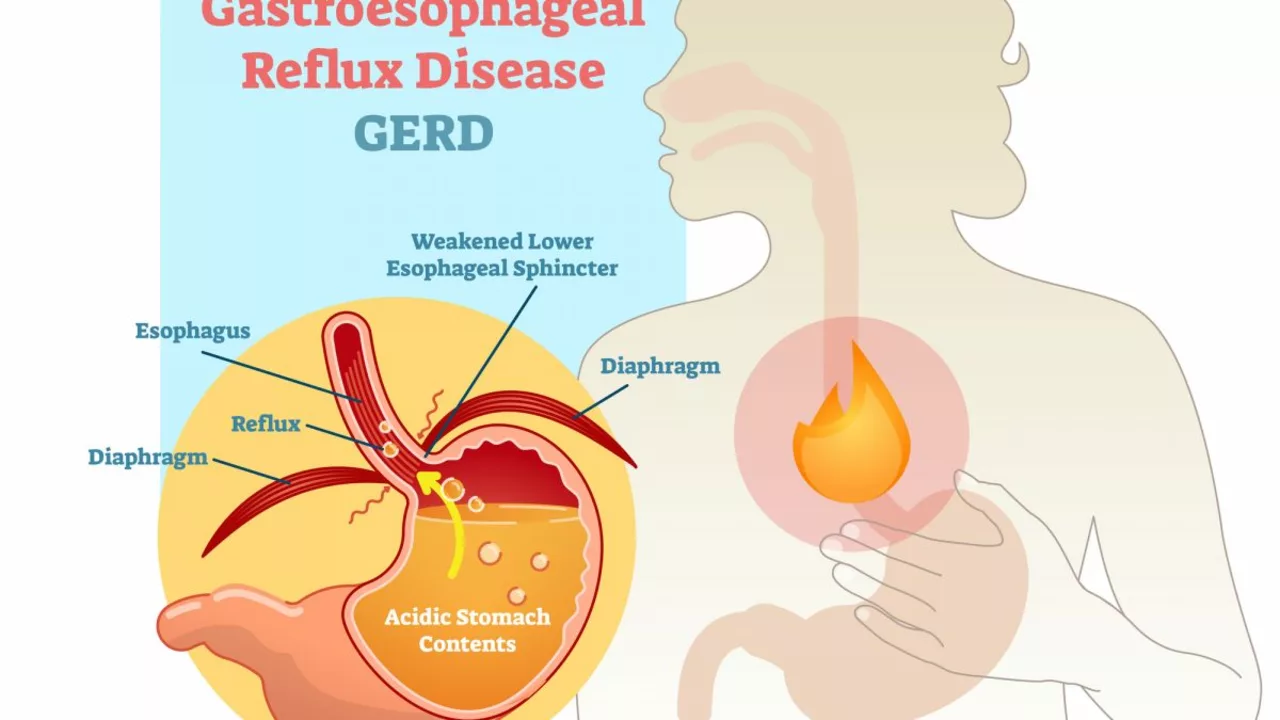
What is Gastroesophageal Reflux Disease (GERD)?
Gastroesophageal Reflux Disease, commonly known as GERD, is a chronic digestive disorder that affects the lower esophageal sphincter (LES). The LES is a ring of muscle located at the entrance of the stomach, and its primary function is to prevent stomach acid from flowing back into the esophagus. When the LES weakens or doesn't close properly, stomach acid can flow back into the esophagus, causing a burning sensation known as heartburn. GERD can lead to more severe complications if left untreated, such as inflammation, ulcers, and even cancer of the esophagus.
Exploring the Link Between Tympanites and GERD
Although Tympanites and GERD are two distinct conditions, they share several similarities and can often coexist in individuals. The excessive gas production and accumulation in the gastrointestinal tract associated with tympanites can increase the pressure on the LES, thus contributing to the weakening of the sphincter and the development of GERD. Conversely, the presence of GERD can exacerbate the symptoms of tympanites by causing an increased production of gas and bloating.
Lifestyle Changes to Manage Tympanites and GERD
One of the most effective ways to manage both tympanites and GERD is to adopt certain lifestyle changes that can help alleviate the symptoms and prevent further complications. Some helpful tips include:
- Eating smaller, more frequent meals throughout the day
- Avoiding trigger foods, such as fatty, spicy, or acidic foods
- Reducing the consumption of carbonated beverages and alcohol
- Quitting smoking, as it can weaken the LES
- Maintaining a healthy weight, as excess weight can put pressure on the abdomen and LES
- Practicing proper posture, especially while eating
Medical Treatment Options for Tympanites and GERD
While lifestyle changes can be highly effective in managing the symptoms of tympanites and GERD, some individuals may require additional medical intervention. Treatment options for tympanites include over-the-counter gas-relief medications, antacids, and in some cases, prescription drugs to regulate bowel movements. On the other hand, GERD can be treated with a combination of antacids, H2 blockers, and proton pump inhibitors. In more severe cases, surgical intervention may be necessary.
When to Seek Medical Attention
Although both tympanites and GERD can often be managed with lifestyle changes and over-the-counter medications, it's important to seek medical attention if you experience persistent or worsening symptoms. Symptoms that may warrant a visit to the doctor include:
- Severe abdominal pain
- Difficulty swallowing or a sensation of food getting stuck
- Unexplained weight loss
- Recurring vomiting or nausea
- Signs of gastrointestinal bleeding, such as blood in the stool or vomit
Conclusion
Understanding the link between tympanites and GERD is crucial in managing these conditions effectively. By adopting lifestyle changes and seeking medical intervention when necessary, sufferers can greatly improve their quality of life and prevent further complications. Remember, a healthy digestive system is essential for overall well-being, so don't hesitate to consult your doctor if you suspect you may be affected by tympanites or GERD.








We can't keep ignoring the fact that bloating and reflux are not just inconveniences; they are warnings that our lifestyle choices have betrayed our bodies. When we gulp carbonated drinks and skip proper chewing, we invite excess gas to crowd the stomach, pushing against the lower esophageal sphincter. This pressure can pry open the valve and let acid storm the esophagus. It’s a moral duty to respect our gut by eating mindfully and steering clear of trigger foods. Moderation and discipline are the true antidotes, not a quick fix of antacids.
Here’s the science you need to know-gas buildup creates intra‑abdominal pressure that directly strains the LES, making it harder for the valve to stay shut. Cutting meals into smaller portions reduces that pressure, while avoiding fizzy drinks cuts the gas at its source. Probiotics can rebalance gut flora, lowering fermentation that produces gas. Elevating the head of the bed adds a mechanical advantage against reflux at night. In short, a few lifestyle tweaks can tame both tympanites and GERD without a pharmacy trip.
It is evident that the pharmaceutical conglomerates conceal the genuine link between abdominal gas and esophageal sphincter failure. Their marketing blinds us to the simple truth that diet, not pills, dictates the pressure dynamics in our gut. By suppressing this knowledge they keep the market for acid reducers thriving.
I understand how overwhelming the symptoms can feel, especially when they disrupt everyday life. The discomfort of a distended belly paired with a burning chest is genuinely distressing. Listening to your body and adjusting meal timing often brings noticeable relief. Gentle walking after meals can also help move gas along. Remember, you are not alone in this struggle, and small adjustments can make a big difference.
Everyone seems to agree that smaller meals help, but in reality the evidence is barely convincing and many patients see no change. The focus on portion size distracts from deeper issues like gut microbiome composition and stress levels that truly drive reflux.
Listen the gut pressure theory is outdated the LES is a complex neuro‑muscular valve that reacts to more than just gas accumulation it also responds to hormonal signals and dietary fat content therefore simple meal splitting is insufficient
Every step you take toward healthier eating is a victory worth celebrating keep experimenting with low‑FODMAP foods you’ll soon notice the bloating easing and the heartburn subsiding
Your description of the LES function is mostly accurate but consider using "lower esophageal sphincter" consistently and adding a comma before "especially" for clarity. Also, "bloating" should be paired with "abdominal distension" when you want a more precise term.
Great summary, thanks!
One might contend that the ontological interplay between corporeal distension and acid reflux epitomizes a microcosmic reflection of existential imbalance, where the body’s internal turmoil mirrors the soul’s perpetual quest for equilibrium.
Oh, look at that, another article ignoring the superior dietary habits of our nation-obviously the solution lies in adopting our traditional cuisine, which, unlike foreign influences, respects the natural harmony of the digestive tract.
From a gastro‑cultural perspective, the etiopathogenesis of tympanites aligns with the Ayurvedic concept of "agni‑vata dysregulation," necessitating a dhatu‑balancing protocol that incorporates herbal carminatives, mindful eating, and seasonal dietary adjustments.
Listen, if you truly want to master the interplay between intra‑abdominal pressure and LES competence, you must first eliminate the myth that carbonated drinks are harmless and replace them with water‑based hydration strategies.
What if the recommendations you read are part of a larger agenda to keep the public dependent on pharmaceutical suppressants, ensuring a steady profit stream for the conglomerates while the true natural remedies remain hidden?
The pathophysiological nexus between gastric distension and sphincteric incompetence is best elucidated through the lens of contemporary gastroenterological phenomenology, wherein biomechanical stressors are quantified alongside neuro‑hormonal feedback loops.
Honestly, they probably don’t want us to know that simple lifestyle tweaks can outsmart the pharma stash 😜💊
The link between gas buildup and acid reflux is simple to understand.
When the stomach fills with gas, the pressure pushes up against the lower esophageal sphincter.
This pressure makes it harder for the sphincter to stay closed.
A closed sphincter stops stomach acid from moving into the esophagus.
When the sphincter opens too much, acid can flow back and cause heartburn.
Eating large meals adds more volume and more gas to the stomach.
Smaller meals reduce the amount of gas that is produced.
Carbonated drinks also add gas directly into the stomach.
Cutting out fizzy drinks therefore lowers the pressure on the sphincter.
Probiotic foods help balance gut bacteria and reduce gas formation.
Walking after a meal moves the gas through the intestines faster.
Raising the head of the bed by a few inches helps keep acid down while you sleep.
If symptoms persist, a doctor can check for other problems like ulcers.
Medication may be useful, but lifestyle changes are the first line of defense.
By following these simple steps you can control both bloating and reflux without relying on pills.