GERD: A Practical Guide to Spotting Symptoms and Finding Relief
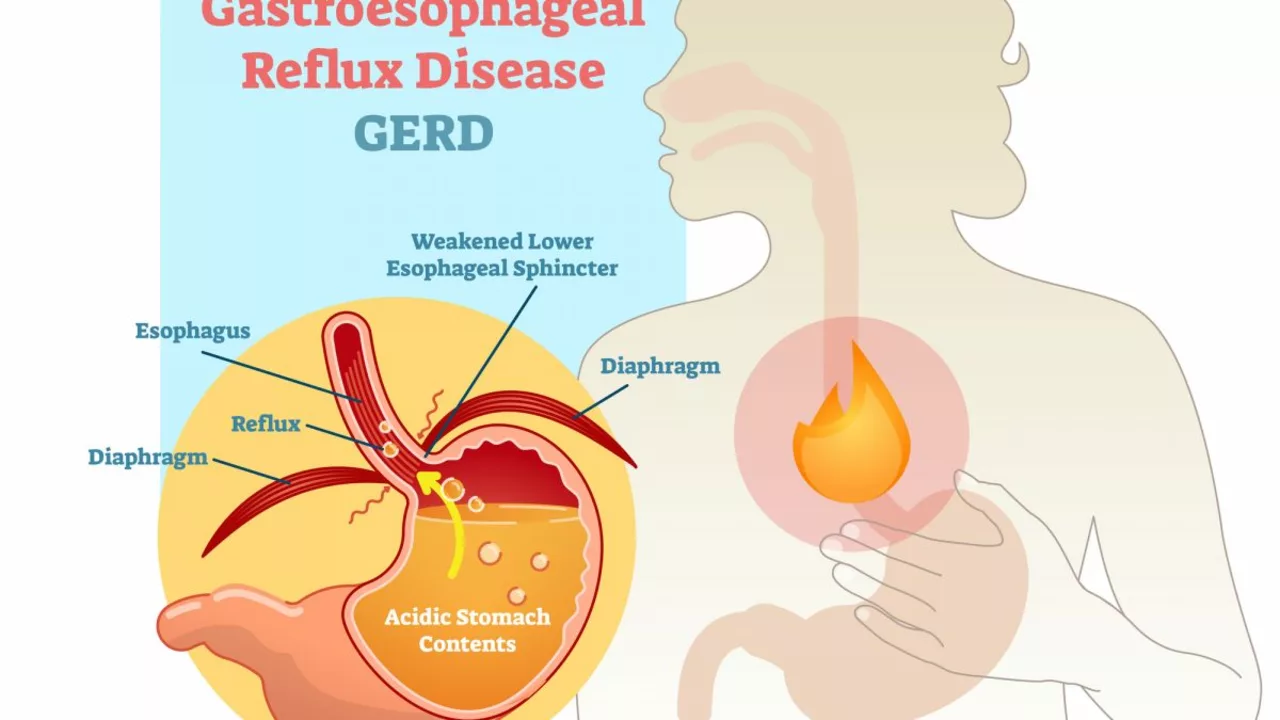
Waking up with a burning chest after a late dinner? That’s a classic sign of GERD (gastroesophageal reflux disease). It happens when stomach acid flows back into the esophagus and irritates the lining. You don’t need to panic, but you do need a plan that mixes simple habits, smarter eating, and the right treatment when needed.
What causes GERD and common signs
GERD starts when the lower esophageal sphincter (LES) doesn’t close well. Other triggers include a hiatal hernia, being overweight, pregnancy, smoking, and some medications. Watch for these common symptoms:
- Heartburn: burning behind the breastbone, often after meals.
- Regurgitation: sour or bitter liquid in the throat or mouth.
- Chronic cough, hoarse voice, or throat clearing.
- Trouble swallowing or feeling food gets stuck.
- Chest pain that’s not clearly heart-related (get checked).
Take immediate medical help if you have severe chest pain, unexpected weight loss, vomiting blood, or trouble swallowing. Those are alarm signs that need urgent evaluation.
Practical diet, lifestyle fixes and treatments
Start with habits you can actually do. Small changes often cut symptoms fast.
- Eat smaller meals and stop eating 2–3 hours before bed. Large or late meals raise reflux risk.
- Sleep with your head raised 6–8 inches or use a wedge pillow. Gravity helps keep acid down.
- Avoid trigger foods: spicy dishes, tomatoes, citrus, coffee, chocolate, peppermint, fried and fatty foods, and alcohol.
- Lose even a little weight if you’re overweight; that often reduces pressure on the stomach.
- Quit smoking and skip tight clothes around the waist.
Diet note: a low-acid, reflux-friendly meal plan can make a big difference. Try bland, low-fat meals with oatmeal, bananas, steamed veggies, lean proteins, and cooked apples. Our site has a low-acid recipes article with seven easy meal ideas if you want ready-made options.
When lifestyle changes aren’t enough, medicines help. Antacids give quick relief for occasional heartburn. H2 blockers (like famotidine) cut acid for hours. Proton pump inhibitors (PPIs) are stronger and used for frequent or severe reflux — take them 30–60 minutes before breakfast for best effect. Talk to your doctor about how long to use PPIs, since long-term use needs monitoring.
If symptoms continue despite treatment, doctors may recommend tests like endoscopy, pH monitoring, or motility tests. In select cases, surgery or endoscopic procedures that strengthen the LES are options.
If you’re unsure where to start, try the lifestyle steps for two weeks and note changes. If heartburn keeps bothering you, see a clinician — persistent reflux can cause complications but is usually manageable with the right approach.
Tympanites and Gastroesophageal Reflux Disease (GERD): Understanding the Link
As a blogger, I've recently been researching the link between Tympanites and Gastroesophageal Reflux Disease (GERD). I discovered that both conditions involve the digestive system and can cause discomfort, but they occur in different areas. Tympanites is the excessive presence of gas in the stomach or intestines, while GERD is a chronic disease where stomach acid frequently flows back into the esophagus. It turns out that certain factors, such as diet and stress, can contribute to the development of both conditions. In my research, I've found it crucial to understand the link between these two disorders to better manage their symptoms and improve overall digestive health.
- View More
- 17