Why People Want Alternatives to Gabapentin for Nerve Pain
Ask around in any pain clinic, and gabapentin absolutely dominates the conversation. It’s the first name tossed out for nerve pain, and a lot of people (doctors and patients) just assume that’s the main ticket to relief. Why do folks start looking for something else? Well, gabapentin's effectiveness varies wildly. For some people, it’s life-changing. For others, it barely makes a dent—or brings along sleepiness, dizziness, or brain fog that makes you want to chuck the bottle across the room. My sister-in-law tried it for burning feet after chemo. She put up with it for two weeks, and then her headaches got too intense. That’s actually pretty common. Upwards of 20% of people report side effects strong enough to quit. Kids have their own stories (my son Evander asks why his friend’s dad loses words and gets silly after his "pills for his back"). It’s enough to make you ask what else is out there. Doctors get stuck, too. Sometimes insurance won’t cover gabapentin unless you’ve failed two other options—or they’ll drop coverage if you complain about side effects. I’ve seen patients wince as they explain, "It just doesn’t work for me anymore." Turns out, you’re not stuck with gabapentin if it lets you down. A half-dozen other medications, plus some lesser-known tricks, might help you feel human again.
Pregabalin: The Sibling Drug and How It Compares
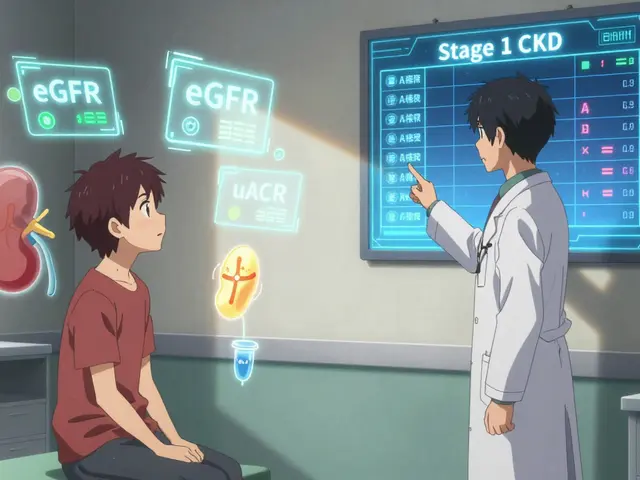
Here's the inside scoop: pregabalin and gabapentin are chemical cousins. Pregabalin (brand name Lyrica) works in a really similar way, dampening the signals jittery nerves send out. But there are a few crucial differences. Pregabalin generally absorbs better (so you need less of it), and it tends to kick in faster than gabapentin. Patients often report fewer wild mood swings and less mental cloudiness. There’s plenty of real-world research behind it—one big trial found pregabalin eased nerve pain by around 50% in about half the patients, which stacked up a little better than gabapentin. But here’s the headache: many insurance companies put pregabalin behind a steep paywall, and it’s more likely to cause weight gain and swelling. I’ve heard stories from diabetes folks who switched to pregabalin and needed to loosen their shoes after a few weeks. Still, if gabapentin failed or left you groggy, plenty of neurologists will try pregabalin next. My daughter Zinnia’s best friend’s grandpa felt like he got his life back after that switch. One quirk: pregabalin is a controlled substance in the U.S., so you’ll jump through a few more pharmacy hoops. Still, it’s far less likely to interact with other meds you might be taking for blood pressure or depression. Not a miracle, but for quite a few with stubborn neuropathy, huge improvement.

The Role of Duloxetine and Other Antidepressants
Sounds weird, right? Antidepressants for nerve pain? Actually, it's one of the best-supported alternatives in the books. Duloxetine (Cymbalta), and sometimes older tricyclics like amitriptyline or nortriptyline, tweak the way your brain processes pain. For folks with diabetic neuropathy, duloxetine has proven to match or even outrun gabapentin in some studies—less tingling, less burning, better sleep. Side effects? You might feel a touch of nausea or dry mouth at the start. One practical perk: if you get both chronic pain and low mood, duloxetine tackles two birds at once. It’s usually started low and ramped up slow to keep headaches, tummy trouble, or jitters at bay. Tricyclics like amitriptyline have been around since the 1960s, and your grandparents might recognize the name. They often work for nighttime pain, but they can bring drowsiness—so plan bedtime early. I’ve seen some folks grow used to the dry mouth and stay on these for years. If your nerve pain comes with trouble sleeping, these meds could be worth a conversation with your doctor. Insurance approval is usually easier, and the generics don’t cost much. Just watch out for grogginess the morning after. And if you have heart issues, talk through the risks—tricyclics aren’t for everyone.
Beyond the Obvious: Less-Known Options Under the Radar
Ever heard of carbamazepine or topiramate for nerve pain? Both started as seizure drugs, and while they’re not front-row favorites, they sometimes sneak onto the list for difficult neuropathy—especially trigeminal neuralgia (that electric-face pain). Carbamazepine’s had decades of street cred for facial nerve shocks, but it can mess with your sodium levels, so you’ll need blood checks. Topiramate may help with burning pain—one friend with fibromyalgia swears by it, even though it sometimes makes soda taste strange (really). Another route that’s catching on is topical treatments. Ever used a lidocaine patch? Easy to slap on, low on side effects, and great for pain in one spot. Capsaicin cream’s an option, too, though the burning at first is rough. My mom literally keeps a tube in her fridge. Some pain docs even use compounded creams mixing several ingredients for more punch. On an experimental note, some small studies suggest certain anti-seizure meds—like lamotrigine—or muscle relaxants (baclofen, tizanidine) can help. It’s very trial-and-error, but if prescriptions keep failing, new approaches keep popping up. Legitimately, it’s worth keeping an eye on what can I take instead of gabapentin, especially if you feel frustrated after the usual attempts. There’s a running tally of trials and real-world tips getting updated every month there.
Lifestyle Changes and Non-Medication Tips Worth Trying
Pills don’t get all the glory—and definitely don’t fix everything. A lot of my friends with stubborn nerve pain found that investing a little effort outside the pharmacy paid off big. Ever try physical therapy? Guided movement—especially with an expert who understands neuropathy—can actually retrain messed-up nerves. Swimming, yoga, or even simple stretching at home can ease stiffness enough to help you sleep. Zinnia’s ballet teacher, who has neuropathy after back surgery, keeps a worn-out foam roller in her classroom. Massage has surprising evidence, especially for diabetic foot pain. Sometimes, the most annoying tip is the one you can actually stick with: cutting down on sugar. Blood sugar swings can make nerve pain worse, so some folks find that a few small food changes go a long way. Next up, mindfulness. It’s not magic, but lowered stress truly does reduce how intensely the brain registers pain. I have an app called Calm on my phone—some days it’s a game changer. Acupuncture divides opinions, but in one 2023 study, around 1 in 4 people described good nerve pain relief after only three sessions. No guarantees, but worth a shot, especially when meds run out of steam. Shoes matter, too. My son Evander’s buddy is obsessed with his Brooks sneakers because the nerve pain in his toes went down when he switched from old, unsupportive shoes. Heat pads and ice packs (rotated through the day) can add relief without drug side effects. If you smoke, quitting is hands-down the best thing you can do to protect your nerves long term—damage just speeds up otherwise.
And here's a stat for the data-lovers: close to 15% of adults over 40 experience nerve pain at some point, according to the latest CDC survey. Out of those, about a third never find total relief with any single medication. Sometimes, it’s all about combining low doses of two or three things—a little pregabalin, gentle PT, solid sleep hygiene—to build your best day. The message from every chronic pain group I know: keep asking. New options are coming out all the time, and you have a right to expect more than just “hope this pill works.”








This article on alternatives to gabapentin is a great read for anyone struggling with nerve pain.
I've found that switching to pregabalin helped my cousin a lot when gabapentin didn't suit him.
It's interesting how different medications can work based on one's unique condition.
Besides meds, the lifestyle changes mentioned like exercise and diet equally play a vital role, right?
Often we overlook such practical tips thinking meds alone can fix everything, but neuropathy is tricky.
Would love to hear your experience if anyone tried duloxetine or other options mentioned here!
Honestly, this article is a bit all over the place. The grammar slips some places, and clarity is lacking when explaining why certain drugs work better.
Also, lumping pregabalin and duloxetine together without highlighting their vastly different mechanisms is careless.
People need clear, precise info, not just a surface overview with fluff.
There should be stronger emphasis on consulting specialists rather than trying to self-medicate based on vague advice.
Additionally, the lifestyle tips are too generic to be genuinely helpful.
I get where you're coming from, but sometimes simple summaries help laypeople get a foothold before diving into complex jargon.
For example, duloxetine is an SNRI and repurposed for nerve pain, which makes sense once you understand its role.
Also, lifestyle changes aren't fluff - small diet and exercise adjustments do improve nerve pain in real life, backed by many studies.
Complex medical info can overwhelm and discourage some patients.
Balance between precision and accessibility is key.
Oh please, let's not sugarcoat it — most alternative medications to gabapentin are either less effective or come with worse side effects.
The pharmaceutical industry is all about pushing newer drugs for profit rather than true patient benefit.
If gabapentin isn't cutting it, chances are you’re chasing a placebo effect with these alternatives.
Don’t fall for the hype; focus on managing expectations instead of endlessly switching meds.
Real talk: pain management isn't some miracle cure; it's about coping.
Anyone expecting a perfect replacement is setting themselves up for disappointment.
I’m really impressed by how this article includes lifestyle changes alongside meds!
For people struggling with neuropathy, that holistic approach is really motivating.
Sometimes we get stuck focusing only on drugs and forget that small steps in exercise, diet, and stress management can lighten the burden significantly.
Hope more resources highlight this balance.
Also, anyone else find a combo of meds plus yoga really helpful?
Trying to keep positive through chronic pain is hard but this kind of info helps.
This discussion is so important because nerve pain can feel isolating.
So many medications have different effects on different people, and personal support matters a lot.
I encourage folks to talk openly with healthcare providers and consider complementary therapies, too.
And yes, lifestyle tweaks like mindfulness and proper sleep hygiene really complement medicine well.
Thanks for stressing a well-rounded approach; it's so often missed.
While I respect the intention behind presenting alternatives to gabapentin, I am skeptical whether any of these so-called options truly provide superior relief.
Pregabalin is just a tweaked version, sharing much of gabapentin’s pharmacology.
Duloxetine’s effectiveness may largely stem from its antidepressant action rather than direct nerve pain relief.
The entire neuropathy treatment paradigm remains opaque and riddled with trial-and-error.
Users might be better served by exploring emerging pain management technologies than traditional meds.
I appreciate all the perspectives here.
From a practical standpoint, people should definitely consult with a neurologist or pain specialist before changing any medications.
Neuropathy varies widely between patients, so what works for one may not for another.
Likewise, lifestyle interventions should accompany rather than replace medical treatments.
Being safe and informed has to be the priority.
:) yeah am trying duloxetine now. it’s been ok not amazing but better than nothing imo.
this article gave me hope to try some other things too!
i also started walking daily and trying to eat healthier :)
hope it helps me in the long run
anyone else have tips like this to share?? 😊
Actually, when considering pharmacodynamics and neurotransmitter receptor affinities, duloxetine’s SNRI profile implies potential modulation of descending inhibitory pain pathways, hence its utility in neuropathic pain management.
The article should have delved deeper into such mechanistic underpinnings rather than providing superficial recommendations.
Moreover, pregabalin’s action on the α2δ subunit of voltage-gated calcium channels deserves more exploration to appreciate why some patients respond more robustly.
Any serious discussion warrants these complexities to weigh options scientifically.
Oversimplification does a disservice to clinical decision-making.
It's honestly frustrating to see people glamorize these alternatives without acknowledging their frequent adverse effects and limited efficacy.
Many patients report dizziness, fatigue, or worse with pregabalin or duloxetine.
One shouldn't be blind to the fact that every alternative comes with its own baggage.
Real talk: managing expectations and preparing for side effects is crucial.
Otherwise, you end up in a revolving door of disappointments.