Automated Dispensing Cabinets (ADCs) are now in over 95% of U.S. hospitals, and many clinics use them too. They’re supposed to make giving out meds safer-no more guessing which pill is which, no more fumbling through drawers. But here’s the truth: ADCs don’t fix errors by themselves. If they’re set up wrong, or staff aren’t trained, they can actually cause more mistakes than they prevent.
One study found that in six out of seven nursing units, error rates went up by over 30% after ADCs were installed. Why? Because nurses were rushing, overriding safety alerts, or pulling the wrong drug because fentanyl and naloxone were placed right next to each other. That’s not a system failure-it’s a setup failure.
What an ADC Actually Does
An Automated Dispensing Cabinet is a locked, computer-controlled box that stores medications in individual doses. It connects to your hospital’s electronic health record (EHR), checks for allergies and drug interactions, and requires a barcode scan before any drug is taken out. Popular models include BD Pyxis MedStation, Omnicell XT, and Capsa Healthcare’s NexsysADC. These systems don’t just hold pills-they track who took what, when, and why.
Modern ADCs have temperature-controlled compartments for insulin, heparin, or other cold-sensitive drugs. They lock out drugs that shouldn’t be in certain units-like keeping high-risk meds out of a general floor unless approved. Some even have voice prompts or biometric login coming soon. But none of that matters if the cabinet is configured like a guessing game.
Why ADCs Can Make Things Worse
The biggest danger isn’t the machine. It’s the override button.
Every ADC has an override function-something that lets staff grab a drug without scanning, even if the system says no. That’s meant for emergencies. But in practice, nurses override 58% of the time in many facilities, according to ISMP audits. Why? Because they’re tired. Because the system is slow. Because they’ve done it before and nothing happened.
One 2017 case at a Midwest hospital showed a patient getting 10 times the right dose of insulin. Why? The nurse hit override because the system flagged the dose as too high-but she didn’t check the patient’s weight or recent labs. The ADC didn’t cause the error. The lack of training and poor override controls did.
Another issue? Look-alike, sound-alike drugs. If you put metoprolol and amiodarone in adjacent drawers, someone will grab the wrong one. And if those drawers aren’t labeled with patient-specific barcodes? You’re gambling.
How to Set Up an ADC Right
Setting up an ADC isn’t like plugging in a printer. It’s a clinical process. Here’s what works:
- Form a team-Pharmacists, nurses, IT, and even unit managers. No one person should decide this alone.
- Map out your meds-Which drugs go where? Keep high-risk drugs (like insulin, heparin, opioids) in locked drawers with double verification. Never put them next to drugs that reverse their effects (like naloxone next to fentanyl).
- Configure overrides-Limit how many times someone can override in a shift. Require a second licensed provider to witness every override. Document the reason every time. No exceptions.
- Use barcode scanning-Every medication you pull must be scanned against the patient’s wristband and the EHR. No shortcuts. Even if you’ve done it 100 times.
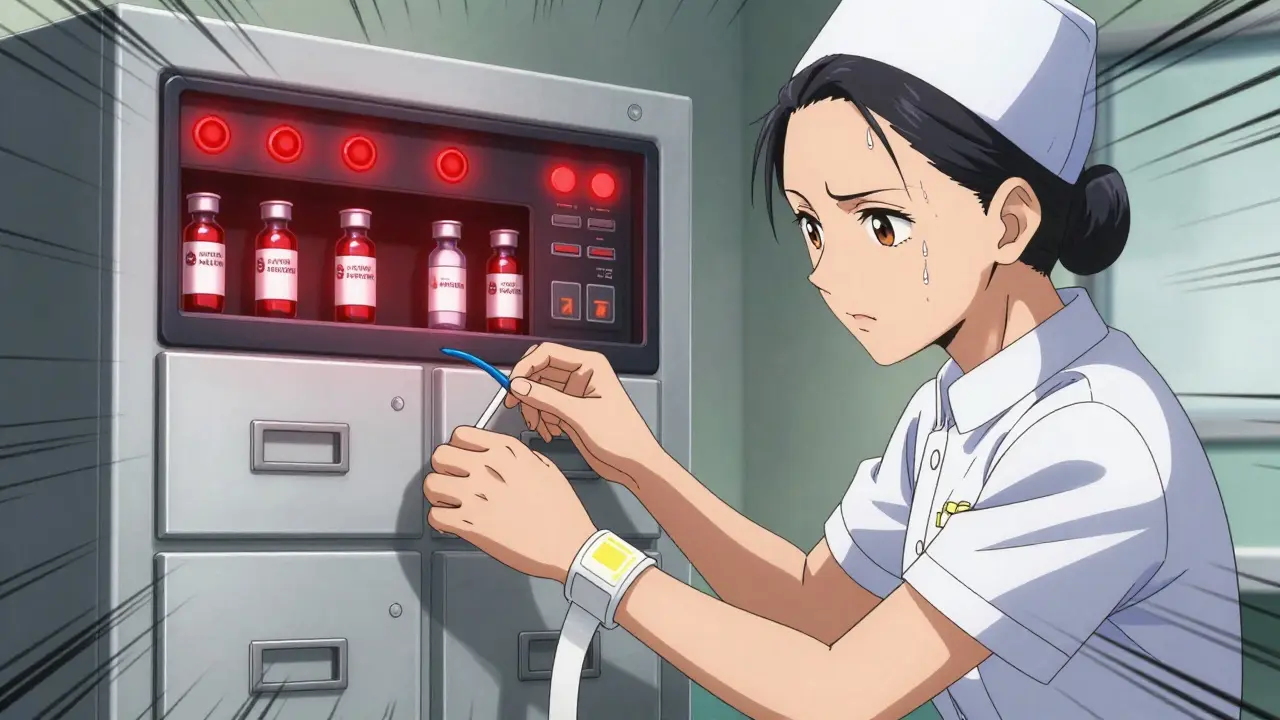
- Label everything-Medications in refrigerated drawers must have beyond-use dates (BUD) clearly marked. No handwritten notes. No stickers peeling off.
- Place it right-Don’t put the ADC near a sink, a window, or a heating vent. Moisture and heat ruin electronics and meds. Keep it in a clean, dry, quiet spot. And yes-keep disinfectant wipes nearby. Pandemics didn’t go away.
Training Isn’t Optional
Most clinics think training means a 30-minute video and a handout. That’s not enough.
ISMP says staff need 4 to 6 weeks of hands-on practice before they’re cleared to use an ADC alone. That includes:
- Scanning practice with fake patient IDs
- Simulated override scenarios
- Learning how to read alerts-not ignoring them
- Understanding why certain drugs are restricted on their unit
At Mayo Clinic, they created unit-specific override lists. For example, the ICU could override for vasopressors, but not for insulin. The med-surg floor? No overrides for opioids at all. That cut override-related errors by 63%.
And don’t forget: if your ADC doesn’t talk to your EHR, you’re missing half the safety net. The system needs to know the patient’s weight, kidney function, allergies, and current meds before it lets you pull a dose. If it doesn’t, you’re just using a fancy locked box.
What to Watch Out For Daily
Even with great setup, mistakes creep in. Here’s what to check every shift:
- Is the drawer you’re using the right one? A nurse once pulled morphine from the fentanyl drawer because the labels were faded.
- Did you scan the patient’s wristband? Not the chart. Not the bed number. The wristband.
- Did you double-check the dose? An ADC can say 5 mg-but if the patient weighs 45 kg, that’s dangerous. Always verify manually.
- Are there any expired or unlabeled meds in the cabinet? If yes, report it. Don’t just move them to the back.
- Did you wash your hands before and after? Studies show 40% fewer contamination risks when staff follow clean-hand protocols near ADCs.
What Happens When You Skip the Rules
There’s a pattern in every ADC-related error I’ve seen:
- Staff were rushed
- They didn’t scan
- They overrode without a second check
- No one reviewed the log afterward
One hospital had 12 near-misses in 3 months because nurses kept overriding insulin alerts. The pharmacy team didn’t monitor logs. No one noticed. Then, a patient went into cardiac arrest. Turned out the dose was 8 times too high.
That’s not a system failure. That’s a culture failure.
ADCs work best when everyone-from the janitor who wipes the cabinet to the chief medical officer-understands that safety isn’t a feature. It’s a habit.
What the Experts Say
Dr. Michael Cohen, former president of ISMP, put it bluntly: "ADCs do not improve safety unless the cabinet’s design and use are planned with attention to patient profiling and other critical factors."
ASHP says the same thing: every facility must have a written plan for how ADCs are used. Not a brochure. Not a PowerPoint. A real, living document that gets updated every time something changes.
And here’s the kicker: only 63% of hospitals follow all nine of ISMP’s Core Safety Processes. That means nearly 4 out of 10 facilities are operating with blind spots.
Final Rule: Don’t Trust the Machine
ADCs are tools. Not babysitters. They can’t replace your brain. They can’t replace your judgment. They can’t replace your hand on the patient’s arm before you give the drug.
Use them. Trust their alerts. But always, always verify.
If you’re not scanning. If you’re not double-checking. If you’re overriding without a witness-you’re not saving time. You’re just gambling.
And in a clinic? There’s no second chance.
Can ADCs reduce medication errors?
Yes-but only if they’re set up correctly. Studies show ADCs can reduce dispensing errors by 15-20% when used with barcode scanning, pharmacist review, and proper override controls. But if overrides are unchecked or staff aren’t trained, error rates can rise by over 30%.
What’s the biggest risk with ADCs?
The override function. When nurses or staff bypass safety checks without proper documentation or a second verification, errors spike. Facilities with unrestricted overrides have 2.3 times more errors than those with strict controls.
Do ADCs need to connect to the EHR?
Yes. Without integration, the ADC can’t check for allergies, drug interactions, or correct dosing based on weight or kidney function. An ADC without EHR access is just a locked cabinet with a screen.
How often should ADCs be audited?
Monthly audits are the minimum. Check for expired meds, unlabeled drugs, override logs, and drawer placement. Pharmacies should review override patterns weekly to spot trends-like one nurse overriding 15 times in a shift.
Are ADCs worth the cost?
For clinics that handle high-risk meds or have frequent medication errors, yes. Units like ICUs and surgical centers see the biggest return. A well-run ADC can prevent just one serious error-like a wrong insulin dose-and pay for itself. But if you’re just using it to save time, you’re missing the point.
What should I do if I notice a safety issue with the ADC?
Report it immediately. Don’t wait. Talk to your pharmacy team. Use your facility’s safety reporting system. Many errors happen because someone saw a problem but didn’t speak up. Your voice can stop the next mistake.




ADCs are a joke if you don’t train people. I’ve seen nurses override like it’s a video game-no consequences, no accountability. It’s not the machine’s fault. It’s the culture. Just give ‘em a badge and a password and call it a day. 😒
I’ve worked in three different hospitals with ADCs, and honestly? The difference between a good setup and a disaster is night and day. At my last job, we had pharmacists sit with every unit for two weeks-teaching them how to read alerts, where to put the high-risk meds, even how to wipe down the cabinet. We cut overrides by 70%. It wasn’t magic. It was consistency. People forget that tech doesn’t fix lazy habits-it just makes them faster. If you skip the training, you’re not saving time, you’re just setting up a ticking bomb. And yeah, the fentanyl/naloxone thing? That’s criminal. One nurse I knew pulled the wrong one because the labels were peeling. She didn’t even notice until the patient started seizing. That’s not an error. That’s negligence wrapped in a barcode.
Also-no one talks about how the cabinets get placed. I’ve seen them right next to the sink. Moisture ruins the scanners. You think the system’s glitching? Nah. It’s just corroded. And don’t get me started on expired meds hiding in the back. If your pharmacy isn’t auditing weekly, you’re not managing safety-you’re just hoping.
At the end of the day, the ADC doesn’t care if you’re tired. It doesn’t care if you’ve been on for 12 hours. It just records what you do. And if you override without a witness? That’s on you. Not the machine. Not the vendor. You.
My advice? Make every override require a second person to type out why they did it. No checkboxes. No dropdowns. Actual typing. It slows you down. And that’s the point.
LMAO I just saw a nurse override an insulin alert and then high-five the guy next to her like they won a bet. 😂 We need cameras on these things. Or at least a public leaderboard of ‘Most Overrides in a Shift.’
Man, I love how this post breaks it down like a clinical playbook. It’s rare to see someone actually talk about the *why* behind the setup-not just the ‘do this’ checklist. The part about placing the cabinet away from heat and sinks? Genius. I’ve seen cabinets literally sweating from humidity, and the screens go fuzzy. It’s like the machine is begging you to stop and fix it. And the EHR integration? If your ADC doesn’t know the patient’s creatinine level, it’s just a glorified vending machine with a panic button. We need to stop treating these like IT equipment and start treating them like life-support systems. Because honestly? They are.
Also-can we just rename ‘override’ to ‘I’m too tired to think’ mode? That’d make people pause before hitting it.
One time I caught a label peeling off a drawer-just a little corner. I reported it. Got a thank you email. Two weeks later? Still there. 😔 We need to stop treating safety reports like paperwork and start treating them like emergencies. If you see a peeling label? Don’t wait. Don’t hope someone else notices. Fix it. Or yell about it. Either way-don’t ignore it.
This. So much this. I’ve been on the floor for 14 years. I’ve seen ADCs go from ‘this is the future’ to ‘why is this so slow?’ But the truth? The future only works if we show up for it. Not just with tech, but with patience. With training. With each other. I wish more people understood that.
adc's r just another way for hospitals to shift blame. nurses override bc they r overworked and underpaid. fix the system, not the cabinet. also why do u need 6 weeks of training? its a box that gives pills. 🤷♂️
Love the breakdown. One thing I’d add: make sure the cabinet’s audit logs are accessible to frontline staff-not just pharmacy. If the nurse can see who’s overriding and why, it creates accountability without needing a committee. We did this at my hospital. Override rates dropped 40% in a month. No lectures. Just transparency.