Every year, millions of Americans take supplements-vitamins, fish oil, turmeric, garlic pills, St. John’s wort, ashwagandha, and more. Many believe these are harmless because they’re ‘natural.’ But here’s the truth: supplements can be just as powerful-and just as dangerous-as prescription drugs. And if your doctor doesn’t know you’re taking them, you’re playing Russian roulette with your health.
Most People Don’t Tell Their Doctors, Even When They Should
A 2018 study found that only 33% of people who take herbal or dietary supplements actually tell their doctors. That number hasn’t budged much in over a decade. Even among people with chronic conditions like diabetes, heart disease, or high blood pressure-those who are on multiple medications-less than half disclose their supplement use. Why? Because most patients assume their doctor doesn’t care. Or worse, they think their doctor will judge them. One patient on Reddit shared: “I took garlic pills for years to lower my blood pressure. Never mentioned it. Then I almost bled out during a minor surgery.” Turns out, garlic thins the blood. Same as warfarin. And when you combine them? Risk of internal bleeding spikes. Another common myth: “It’s just a supplement, not medicine.” But St. John’s wort? It’s used to treat depression. Turmeric? It affects liver enzymes. Ashwagandha? Can lower blood pressure and blood sugar. These aren’t harmless teas. They’re bioactive compounds with measurable effects on your body.What Happens When You Don’t Disclose
The risks aren’t theoretical. They’re documented in peer-reviewed journals and emergency room reports. - St. John’s wort cuts the effectiveness of birth control pills by up to 60%. Women have gotten pregnant while on the pill-because they were also taking this “natural mood booster.” - Ginkgo biloba and garlic both interfere with blood thinners like warfarin. Patients have ended up in the ER with brain bleeds after minor falls. - Green tea extract has been linked to liver damage in people taking statins. - Calcium supplements can block absorption of thyroid medication if taken at the same time. - Iron supplements make antibiotics like ciprofloxacin useless. The FDA doesn’t test supplements for safety or effectiveness before they hit shelves. That’s because of the 1994 Dietary Supplement Health and Education Act (DSHEA). The burden is on the FDA to prove something is dangerous after it’s already sold. That’s like letting a car roll off the assembly line without brakes-and only pulling it back if someone crashes.Doctors Aren’t Always Asking-But They Should Be
Here’s the uncomfortable truth: most doctors don’t ask about supplements. A 2021 survey found only 27% of physicians felt adequately trained to discuss them. Many assume patients will volunteer the info. But patients rarely do. One study showed that when doctors simply asked: “Do you take any vitamins, herbs, or supplements?”-disclosure jumped from 33% to 78%. That’s not magic. That’s just asking. The problem isn’t just ignorance. It’s time. A typical doctor’s visit lasts 15 to 20 minutes. Blood pressure, cholesterol, new symptoms-those get priority. Supplements? They’re an afterthought. Unless you bring them up.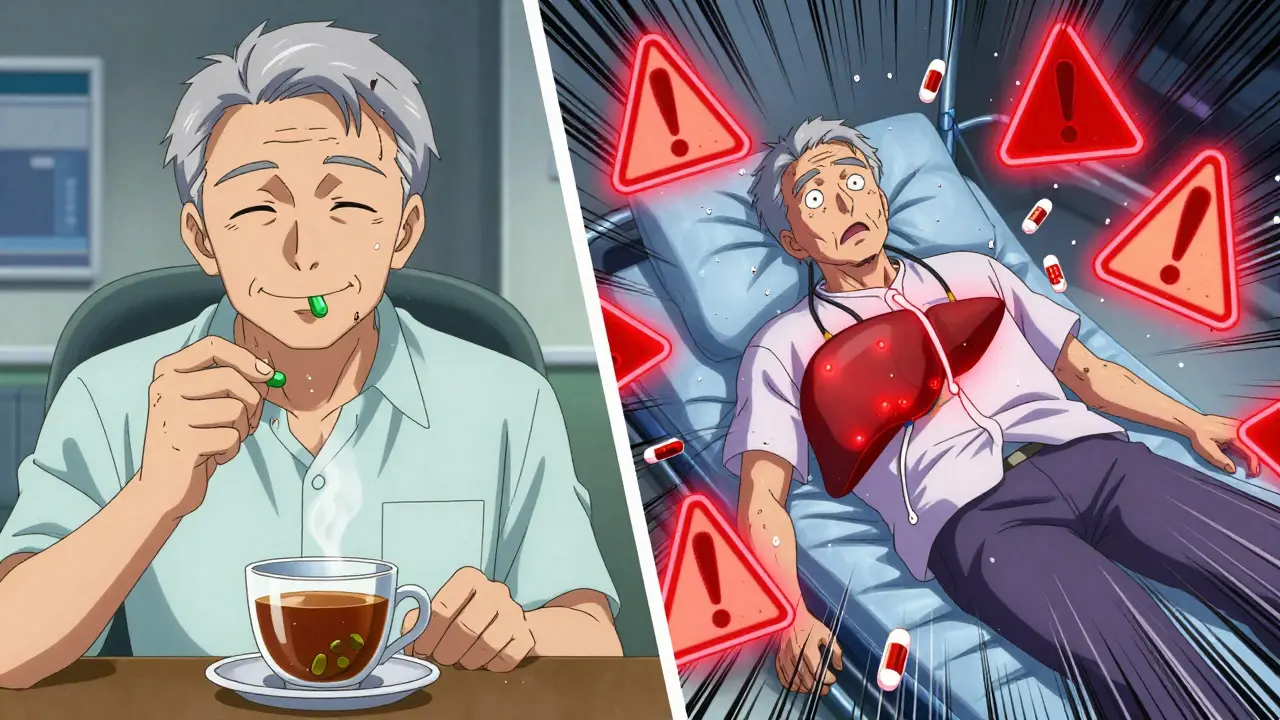
How to Talk to Your Provider-Without Getting Judged
You don’t need to be an expert. You don’t need to defend your choices. Just be honest and prepared.- Bring the actual bottles. Don’t rely on memory. Labels list exact ingredients and dosages. Your doctor can’t guess what’s in that unlabeled capsule.
- Use simple language: “I take this for X. I didn’t think it mattered. Can you tell me if it’s safe with my other meds?”
- Don’t say “I’m taking this because my friend says it works.” Say: “I’ve been taking this for six months. I want to make sure it’s not hurting me.”
- If your provider dismisses you, ask: “Is there any research showing this interacts with my medications?”
What Your Provider Needs to Know
It’s not just about pills. It’s about everything:- Herbs: turmeric, ginger, echinacea, milk thistle, ginseng
- Minerals: magnesium, zinc, calcium, iron
- Vitamins: D3, B12, C, E
- Probiotics and prebiotics
- Protein powders and amino acids
- Essential oils taken internally
- Teas labeled as “medicinal” (like dandelion root tea for liver support)

What’s Changing-and What You Can Do Now
The tide is turning. The American Medical Association now requires medical schools to teach supplement interactions. The FDA added 70 new ingredients to its safety watchlist between 2020 and 2023. Apps like MyMedList help patients track everything they take-and share it with providers in one click. But none of this matters if you stay silent. Your provider isn’t trying to shut down your wellness habits. They’re trying to keep you alive. If you’re taking something to feel better, why risk making yourself sicker?Next Steps: What to Do Before Your Next Appointment
1. Take inventory. Open your medicine cabinet. Write down every supplement, herb, and tea you take daily or weekly. 2. Check labels. Note the exact name, dose, and manufacturer. Many products hide ingredients under “proprietary blends.” 3. Bring the bottles. Don’t rely on memory. Photos of labels aren’t enough-your doctor needs to see the actual product. 4. Ask directly. At the start of your visit: “I’d like to talk about what I’m taking outside of prescriptions. Is that okay?” 5. Follow up. If your provider says “It’s fine,” ask: “Is there any reason I should stop or change it?” You don’t need to stop your supplements. You just need to know if they’re safe with your current health situation.Frequently Asked Questions
Do I really need to tell my doctor about vitamins and fish oil?
Yes. Even common supplements like fish oil, vitamin D, or multivitamins can interact with medications. Fish oil can thin your blood, which is dangerous if you’re on warfarin or aspirin. High-dose vitamin D can raise calcium levels and damage your kidneys if you have kidney disease. Your doctor needs to know everything.
What if my doctor says supplements are useless?
That’s their opinion. Your job isn’t to convince them-they’re there to keep you safe. If they dismiss you, say: “I’m not asking if it works. I’m asking if it’s safe with my other meds.” If they still refuse to engage, consider finding a provider who takes integrative health seriously. Your health isn’t negotiable.
Can herbal remedies cause liver damage?
Yes. Green tea extract, kava, comfrey, and high-dose niacin have all been linked to liver injury. The FDA has issued warnings on over 170 ingredients with known safety risks. Many of these are sold in stores as “natural energy boosters” or “detox teas.” If you’re taking anything labeled for liver support, talk to your doctor-your liver may be under stress already.
Why don’t supplement labels say they might interact with my meds?
Because the law doesn’t require it. Supplement labels must say: “Not evaluated by the FDA. Not intended to diagnose, treat, cure, or prevent any disease.” That’s it. No interaction warnings. No dosage limits. No safety data. That’s why you need to tell your doctor-they’re the only ones who can connect the dots.
I’m on Medicare. Should I be extra careful?
Absolutely. Over two-thirds of Medicare beneficiaries take supplements. Many are on five or more prescriptions. The risk of dangerous interactions is highest here. A 2023 study found that seniors who disclosed supplement use had 40% fewer emergency visits related to drug reactions. Don’t assume your pharmacist or doctor knows what you’re taking. Tell them.





Thank you for this!! 🙏 I just started taking ashwagandha for stress and had no idea it could mess with my blood pressure meds. I’m bringing my supplement bottles to my next appointment-no more guessing games. You’re right, it’s not about judgment, it’s about safety.
The FDA’s hands are tied because of DSHEA. This law was written by supplement industry lobbyists in 1994 to avoid regulation. It’s not an accident that dangerous products flood the market. It’s policy.
You think your doctor cares? My GP laughed when I asked about turmeric and my anticoagulants. Said, ‘It’s just spice.’ I stopped trusting him after that. You’re not being paranoid-you’re being smart.
They don’t want you to know this, but supplements are the only thing keeping you alive while Big Pharma sells you overpriced pills with side effects that make you worse. The whole system is rigged. They’re scared you’ll figure out you don’t need their drugs. Green tea extract? That’s just nature fighting back against synthetic chemicals. 🤫
YES. I used to think fish oil was ‘just for heart health.’ Then I got a nosebleed that wouldn’t stop after my knee surgery. Turns out, it was the fish oil + aspirin combo. Now I list everything on a sticky note and hand it to my doctor before they even say ‘hello.’ Game changer.
Why are we letting the government regulate our health? This is America. If I wanna take 10 garlic pills and a gallon of turmeric tea before my colonoscopy, that’s my right. They just don’t want you to be healthy without paying them. Wake up.
So... doctors don't know stuff? Wow. Mind blown. Next they'll tell me water is wet.
I’ve been taking magnesium for sleep for three years… never told my doctor. Now I’m wondering if that’s why my blood pressure spiked last month. Maybe I should’ve just… said something? 🤔
Doctors should ask. Patients should tell. Simple. No drama.
So let me get this straight… you’re telling me that the same people who sold me ‘detox tea’ that made me vomit for 3 days are now telling me ‘natural’ means safe? 😭 This whole thing is a scam. I’m done. I’m switching to tea made from crystals and moonlight. It’s at least honest about being useless.
For anyone new to this: start small. Write down everything-even the gummy vitamins. Bring them in a ziplock bag. Most doctors will be glad you did. You’re not being annoying-you’re being responsible. Your future self will thank you.
So… the government lets companies sell ‘medicinal’ teas with no testing… but I can’t buy a vape without a PhD? Hmm. Yeah, that makes sense. Totally logical. 😒
It is regrettable that the prevailing cultural paradigm has led to the commodification of wellness as a market-driven enterprise, wherein bioactive botanicals are marketed under the false pretense of benignity. The regulatory vacuum created by DSHEA constitutes a profound failure of public health governance. One must, therefore, exercise epistemic vigilance and demand evidence-based discourse in lieu of anecdotal assertions. The onus is not upon the patient to educate the physician; rather, the physician must be trained to interrogate the pharmacological profile of all ingested substances, regardless of their perceived innocuousness.
Wow. So… I’m supposed to tell my doctor I take vitamin C? Like, the stuff in orange juice? This is ridiculous. I’m not going to carry around my supplement bottles like I’m at a drug deal.