What if taking your pill 30 minutes earlier or later could mean the difference between feeling fine and ending up in the hospital? It’s not a hypothetical. For many medications, timing isn’t just a suggestion-it’s a critical part of how safe and effective the drug is.
Why Your Body Has a Clock
Your body runs on a 24-hour cycle called the circadian rhythm. It controls when you feel sleepy, when your blood pressure rises, when your liver processes toxins, and even when your stomach is most ready to absorb medicine. These rhythms aren’t random-they’re deeply wired into your cells, influenced by light, food, and even your sleep schedule. When you take a medication, your body doesn’t treat it the same way at 8 a.m. as it does at 8 p.m. Liver enzymes that break down drugs can be twice as active at night. Kidneys filter differently depending on the time of day. Blood flow to your stomach changes. All of this affects how much of the drug actually reaches your bloodstream and how long it stays there. This is the foundation of chronotherapy: using your body’s natural clock to make medicines work better and hurt less. It’s not new-scientists have known about it since the 1970s-but it’s only now becoming part of everyday care.Medications That Need Exact Timing
Not all drugs care when you take them. A regular ibuprofen for a headache? Probably fine anytime. But some medications have narrow windows where timing matters a lot. Insulin is one of the most dangerous if mistimed. Taking rapid-acting insulin too early before a meal can drop your blood sugar dangerously low. Waiting too long can spike it. Studies show mistimed insulin leads to hypoglycemia in about 22% of cases. Anticoagulants like warfarin or apixaban are another high-risk group. Even a 2-hour delay can increase bleeding risk by up to 37%. That’s because these drugs need to stay at a steady level in your blood. Too much? Risk of internal bleeding. Too little? Risk of stroke. Chemotherapy drugs are timed down to the minute in hospitals. Deviating more than 30 minutes from the schedule can cut effectiveness by 15-20%. Why? Cancer cells divide at specific times, and some chemo agents only work when those cells are most vulnerable. Morphine for severe pain also has a tight window-10 to 15 minutes. Outside that, pain control drops fast, and side effects like dizziness or nausea spike.Medications That Work Better at Night
Some drugs don’t just tolerate nighttime dosing-they actually work better. Statins, like atorvastatin or rosuvastatin, are a prime example. Cholesterol production in your liver peaks between midnight and 4 a.m. Taking statins at night means the drug is at its strongest when your body is making the most cholesterol. Studies show this boosts LDL (bad cholesterol) reduction by 15-20% compared to morning doses. ACE inhibitors and ARBs for high blood pressure also work better at night. The MAPEC study found that taking these medications before bed reduced cardiovascular events by 29% compared to morning dosing. Why? Blood pressure naturally dips at night, and these drugs help maintain that dip, reducing strain on your heart and kidneys. Beta-blockers for heart conditions, like metoprolol, are another. Nurses in cardiac units report a 40% drop in post-surgery atrial fibrillation when patients take them at night-likely because heart rate and stress hormones peak in the early morning.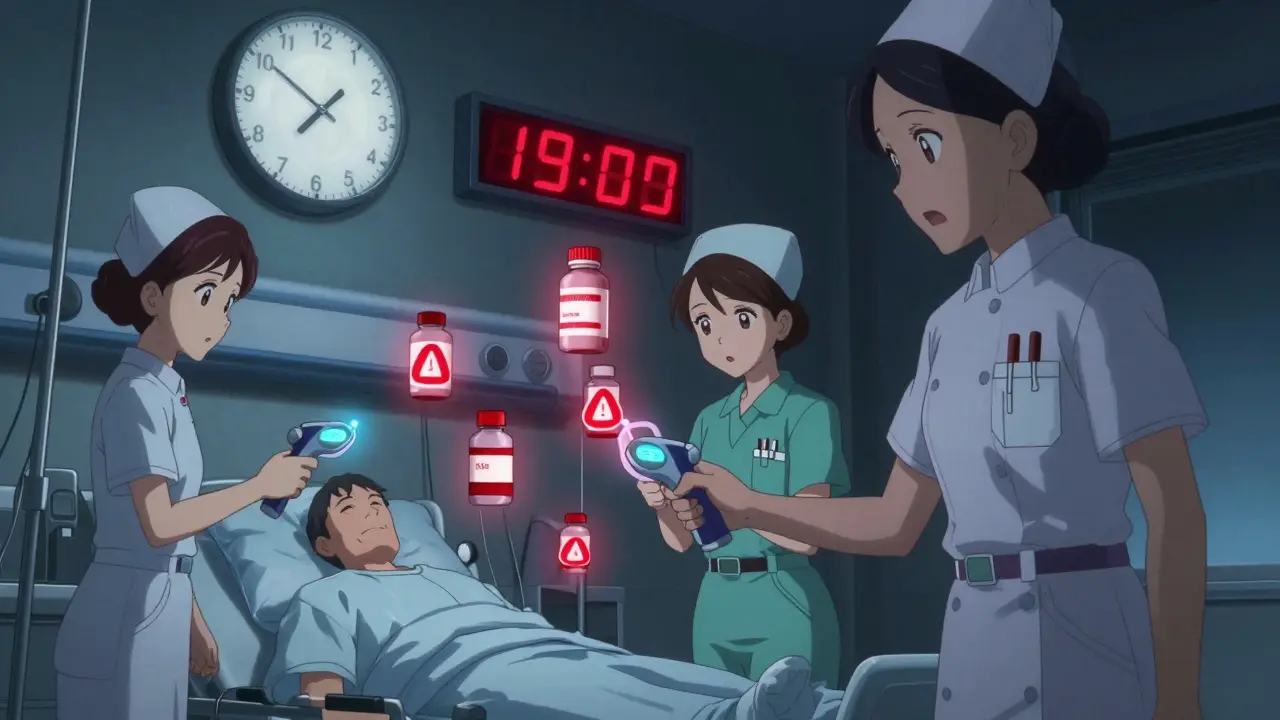
When Timing Doesn’t Matter (Much)
You don’t need to stress over every pill. Some medications are forgiving. Hydrochlorothiazide, a common water pill for high blood pressure, can be taken up to 12 hours off schedule with little effect. It’s a mild diuretic, and your body adjusts easily. Thyroid meds like levothyroxine need to be taken on an empty stomach, but the exact hour isn’t as critical as consistency. Taking it at 7 a.m. every day is better than switching between 6 a.m. and 9 p.m. Antibiotics like amoxicillin are often taken every 8 or 12 hours, but a 1-2 hour variation won’t ruin the course. The key is finishing the full prescription, not hitting the clock perfectly.Why People Miss Their Timing
Even when people know timing matters, they still mess it up. Why? - Work schedules: A nurse working night shifts can’t take her morning blood pressure pill at 8 a.m. if she’s asleep until 2 p.m. - Interruptions: In hospitals, a single interruption during a med pass increases error risk from 39% to 61%. At home, phone calls, kids, or a doorbell can throw off your routine. - Low health literacy: A survey of 1,200 patients found 68% didn’t stick to their timing schedule. Of those, 74% had trouble understanding instructions. - Complex regimens: Taking 10 different pills at different times? It’s easy to mix them up.How to Get It Right
You don’t need a PhD to manage timing. Here’s what works:- Use a pill organizer with time labels-not just morning/night, but 7 a.m., 1 p.m., 8 p.m.
- Set phone alarms for each dose. Label them clearly: “Warfarin-DO NOT SKIP” or “Statins-Take at Bedtime.”
- Ask your pharmacist: “Which of my meds need exact timing?” They can flag the high-risk ones.
- Keep a simple log: A notebook or notes app with checkmarks for each dose. It helps you spot patterns.
- Don’t double up: If you miss a dose, don’t take two later. Call your doctor instead.









I never realized how much my body's clock affects meds until I started tracking my insulin times. Turns out, taking it 20 mins late after dinner meant I was crashing by 11 p.m. every night. Now I set two alarms-one for dinner, one for the shot. Life’s been so much smoother.
Also, weirdly, my anxiety meds work way better at 9 p.m. than 8 a.m. I thought it was placebo, but now I get it-circadian rhythms are real.
Why don’t more doctors talk about this?
THIS. 🙌 I’ve been telling my grandma for years to take her statins at night and she finally listened-now her cholesterol is down 22% and she’s not on the edge of a heart attack anymore 😭
Also, her BP meds? Nighttime. Big difference. She says she sleeps better too. 🌙💊
Y’all need to stop treating meds like candy. Timing matters. A LOT. Talk to your pharmacist. Please.
Statins at night is solid science but the real issue is adherence not timing. Most people forget meds entirely. A pill organizer with alarms is the bare minimum. No one needs a PhD to do this. Just consistency. And if you’re on warfarin don’t wing it. INR tests exist for a reason.
Also the 37% bleeding risk from a 2-hour delay? That’s from a 2019 JAMA study. Cite your sources.
And yes chronotherapy is real but it’s still underutilized because healthcare is broken not because the science is weak
I love how this post doesn’t just scare people but gives practical solutions. Pill organizers, alarms, talking to pharmacists-these are small things that make a huge difference.
I used to mix up my thyroid med and blood pressure pills and ended up dizzy for weeks. Now I color-code everything. Red for morning, blue for night. It’s silly but it works.
Also, if you’re overwhelmed, just pick one high-risk med to nail first. Don’t try to fix everything at once. Progress not perfection.
People are dying because they think a pill is a pill. This isn’t just about convenience-it’s about life or death. Warfarin isn’t aspirin. Insulin isn’t vitamin D. And yet half the people I know take their meds when they remember, if they remember.
It’s not ignorance. It’s laziness wrapped in denial.
And yes I’ve seen people get admitted because they skipped a dose ‘because they felt fine.’ You don’t feel fine when your kidneys fail because you thought timing didn’t matter.
My mom’s on 11 meds. Some she takes at the same time every day, some she forgets. I made her a little chart with pictures-pills, clocks, even emojis for when to take them. She’s 78 and doesn’t read well but she gets the pictures.
She started taking her ACE inhibitor at night like the study says-and now she doesn’t wake up gasping for air at 3 a.m. anymore.
It’s not about being perfect. It’s about being kind to your body. And asking for help when you need it.
If you’re reading this and overwhelmed? You’re not alone. Start with one pill. One alarm. One day.
Chronopharmacology as a clinical discipline remains epistemologically marginalized despite overwhelming circadian pharmacokinetic evidence. The pharmacodynamic variance across diurnal phases is not merely statistical-it is ontologically significant. The liver’s CYP450 enzyme expression, modulated by CLOCK/BMAL1 transcriptional oscillations, exhibits a 2.3-fold amplitude differential between 06:00 and 02:00-yet clinicians still prescribe on a flat-time paradigm.
Moreover, the FDA’s 2022 review of 17 new drug applications with chronopharmacological data represents a paradigmatic shift, yet implementation remains hamstrung by institutional inertia, not scientific uncertainty. The problem is not the data-it is the epistemic hierarchy of clinical practice that privileges convenience over precision.
Personalized chronotherapy via genomic biomarkers (e.g., PER3 variants) will not be adopted until the healthcare system abandons its 19th-century dosing models.
And yes I know this sounds like jargon. But if you don’t understand it, ask. Or read. Or stop pretending timing doesn’t matter.
Bro this changed my life. I used to take my metoprolol in the morning and feel like I was gonna pass out by noon. Started taking it at 9 p.m. now I sleep like a baby and my heart rate’s stable. No more panic attacks. 🙏
Set 3 alarms. One for meds. One for water. One for ‘did I actually take it?’
You got this. One pill at a time.