Anticholinergic Burden Calculator
Medication Selection
Current Medications
Anticholinergic Burden Score
Total ACB Score:
0
Important Information
ACB scores indicate cumulative anticholinergic effects. A score of 3+ increases dementia risk by 54% over 7 years (per 3,400+ adult study).
Never stop medications abruptly. Always consult your doctor before making changes.
When doctors prescribe tricyclic antidepressants (TCAs) like amitriptyline or nortriptyline, many don’t realize they’re handing patients a hidden risk-anticholinergic burden. This isn’t just about dry mouth or constipation. It’s about memory loss that looks like dementia, heart rhythms that turn dangerous, and side effects that stick around long after the drug is stopped. For people over 50, especially those on multiple medications, this burden can quietly erode health in ways that are easy to miss-and hard to reverse.
What Is Anticholinergic Burden?
Anticholinergic burden is the total effect of all the medications in your system that block acetylcholine, a key chemical in your brain and body. Acetylcholine helps with memory, attention, digestion, bladder control, and even heart rhythm. When drugs block it, things start to slow down or go wrong. Tricyclic antidepressants are among the strongest offenders. They were developed in the 1950s to treat depression, and they work by boosting serotonin and norepinephrine. But they also block muscarinic receptors-those are the ones that respond to acetylcholine. That’s why they come with side effects like blurred vision, dry mouth, trouble peeing, and confusion. These aren’t just annoyances. They’re signs of a deeper problem. To measure this, doctors use tools like the Anticholinergic Cognitive Burden (ACB) Scale. On this scale, TCAs like amitriptyline and nortriptyline get the highest score: 3. That means they’re classified as having definite high anticholinergic activity. Even one pill a day can push your total ACB score into the danger zone. A score of 3 or higher is linked to a 54% higher risk of dementia over seven years, according to a major study of over 3,400 adults over 65.Why TCAs Are Riskier Than Other Antidepressants
Modern antidepressants like SSRIs (sertraline, escitalopram) and SNRIs (duloxetine, venlafaxine) barely touch acetylcholine. Most have an ACB score of 0 or 1. TCAs? Always 3. That’s not a small difference-it’s a massive gap in safety. Take amitriptyline. It’s often used for depression, nerve pain, or sleep issues. But it’s also one of the most anticholinergic drugs on the market, alongside over-the-counter sleep aids like diphenhydramine (Benadryl) and bladder meds like oxybutynin. Many patients don’t realize they’re stacking these together. A 70-year-old on amitriptyline for pain, diphenhydramine for sleep, and oxybutynin for incontinence might have an ACB score of 9. That’s three times the threshold for high risk. A 2022 survey by the National Council on Aging found that 68% of adults over 65 taking TCAs reported at least two troubling anticholinergic side effects. Nearly one-third said their memory problems were bad enough to consider quitting the drug.Cognitive Risks: Mimicking Dementia
One of the most dangerous aspects of anticholinergic burden is how easily it mimics dementia. Patients forget names, lose focus, get confused in familiar places. Family members assume it’s Alzheimer’s. Doctors order brain scans and memory tests. But the real culprit? A medication they’ve been on for months-or years. Clinicians on Reddit’s r/psychiatry have shared case after case where patients diagnosed with early dementia turned out to have reversible cognitive decline from amitriptyline. Once the drug was tapered off, their memory improved within weeks. Some returned to near-normal function. The problem? Many don’t make the connection. The National Institute for Health and Care Excellence (NICE) warns that anticholinergic drugs can lead to false diagnosis of dementia. That’s not just a misstep-it’s a tragedy. People are told they have a degenerative brain disease when what they really need is a medication review. Research in Age and Ageing (2023) showed that after a structured deprescribing program, older adults saw their ACB scores drop by 4.2 points on average. Their Mini-Mental State Examination (MMSE) scores-the standard test for cognitive function-went up by 2.7 points. That’s the difference between needing help with bills and managing them independently.
Cardiac Risks: When the Heart Can’t Keep Up
It’s not just the brain. TCAs mess with the heart, too. They act like class 1A antiarrhythmics-drugs meant to treat irregular heartbeats. But unlike those, TCAs aren’t given with careful monitoring. They slow down the heart’s electrical signals, prolonging the QT interval and widening the QRS complex. At therapeutic doses, amitriptyline can lengthen QRS by 10-25%. In overdose, it can jump to 50%. That’s a recipe for torsades de pointes-a life-threatening arrhythmia. Studies show TCAs carry about three times the risk of arrhythmias compared to SSRIs. Amitriptyline specifically increases QT prolongation risk by 2.8 times compared to sertraline. For someone with existing heart disease, high blood pressure, or an older heart, this isn’t just a side effect-it’s a red flag. Patient stories back this up. One member of the Mended Hearts support group described how, after just three weeks on amitriptyline for depression, they started having palpitations and dizziness. An ER visit revealed dangerous QT prolongation. They were hospitalized. The drug was stopped. Their heart rhythm returned to normal.Who Should Still Take TCAs?
This isn’t a blanket ban. TCAs still have a place. For people with treatment-resistant depression-those who’ve tried at least three other antidepressants without success-they can be effective. They’re also one of the few drugs proven to help with certain types of chronic nerve pain, like diabetic neuropathy or postherpetic neuralgia. But even then, they shouldn’t be the first choice. SNRIs like duloxetine work almost as well for pain and depression, with an ACB score of 0 or 1. Cognitive behavioral therapy, physical therapy, and non-drug pain management techniques are safer first steps. The key is this: TCAs should only be used when other options have failed, and only after a full review of all medications. For anyone over 65, the Beers Criteria-used by doctors across the U.S.-says TCAs are potentially inappropriate unless the benefits clearly outweigh the risks.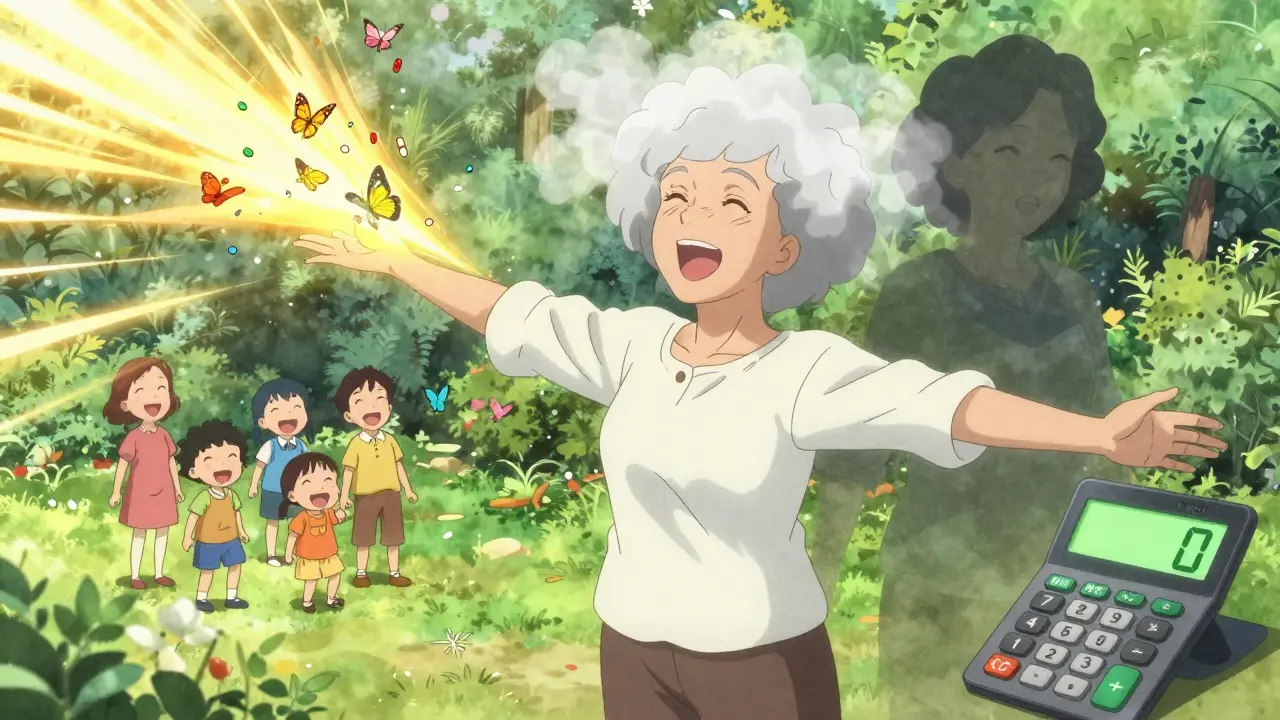









ACB score of 3? That’s not a suggestion-it’s a red flare. I’ve seen it in my mom: forgetfulness, confusion, then the dementia diagnosis. Turned out it was amitriptyline. Tapered off. Three months later, she remembered her own birthday. This isn’t theoretical. It’s clinical tragedy wrapped in a prescription bottle.
Doctors need to stop treating TCAs like harmless relics. They’re not. They’re cognitive landmines.
okay but like… i had no idea diphenhydramine counted?? i’ve been taking benadryl for sleep since college 😅 and my grandma’s on oxybutynin and amitriptyline?? like… we’re all just stacking these things like legos??
my aunt thought her memory was ‘just aging’-turns out her ACB was 8. she cried when she found out it could be reversed. like… why isn’t this on every med bottle??
I’m a nurse. I’ve seen this over and over. Elderly patient comes in with memory issues. Family thinks dementia. We check meds. Boom-three anticholinergics. One’s a TCA. We pull them. Three weeks later, they’re asking about their grandkids’ names again.
It’s not magic. It’s pharmacology. But nobody teaches this in med school anymore. Or if they do, nobody listens.
Why are we still prescribing these like they’re 1985?
This is why Western medicine is broken. You people treat drugs like candy. In India, we know the body better. Ayurveda has been warning about chemical imbalances for 5,000 years. Now you’re blaming a 70-year-old’s memory loss on a pill? Pathetic.
Stop blaming the medication. Blame the weak willpower. Eat turmeric. Meditate. Stop being soft.
Consider this: acetylcholine is not merely a neurotransmitter-it is the metaphysical bridge between intention and memory, between the will and the body’s silent symphony. When we pharmacologically silence it with synthetic blockers, we don’t just disrupt neural pathways-we sever the soul’s connection to its own continuity.
TCAs are not just drugs; they are modern-day alchemical instruments, turning human consciousness into brittle glass. The mind, once fluid, becomes a fossilized echo of itself. We mistake this for aging. We call it ‘normal.’ But normal is the lie we tell ourselves to avoid confronting the violence of our pharmacological arrogance.
And yet, the system persists. Because profit > presence. Because convenience > consciousness. Because we have forgotten how to be human in a world that medicates everything except the wound of disconnection.
My dad was on nortriptyline for 12 years for back pain. He started forgetting where he parked his car. Then he forgot my name for two days. We thought it was early Alzheimer’s. We were devastated.
His new doctor pulled him off it. Six weeks later, he remembered my wedding. He cried. I cried.
Don’t wait for the diagnosis. Ask for the ACB score. It’s that simple.
Anticholinergics are the silent vampires of geriatric care-sucking the warmth from memory, the rhythm from the heart, the spark from the soul… and nobody notices until the candle’s guttering out and the room’s too dark to see the wick.
They’re not side effects-they’re soul erosion.
And we’ve normalized it.
Like calling a funeral a ‘service.’
Like calling a slow death ‘aging.’
Wake up.
It’s not inevitable.
It’s industrial.
So let me get this straight. We’re going to stop using cheap, effective meds because some PhDs ran a study? We’re replacing them with $300/month SSRIs? And you want me to believe this isn’t Big Pharma pushing their overpriced junk?
My grandpa lived to 92 on amitriptyline. He never had dementia. Coincidence? Maybe. But I’m not letting some algorithm scare me off a drug that works.
i am from india and my aunty took amitriptyline for depression… she forgot to turn off the stove twice… we stopped it… she is fine now… thank you for this post… i did not know it was called anticholinergic burden… now i can explain to my family…
thank you.
As a geriatric nurse practitioner, I can confirm: the data is overwhelming. TCAs are not appropriate first-line agents for patients over 50. Period.
But here’s what’s missing from this conversation: access. Many patients can’t afford CBT-I. They can’t get referrals for physical therapy. They’re stuck with what’s in the formulary-and that’s often amitriptyline because it’s $4 at Walmart.
We need policy change, not just patient education.
Let’s fix the system, not just blame the prescribers.