Every year, over 250,000 medication errors happen in U.S. nursing homes - and most go unreported. For seniors taking five or more medications, the risk isn’t just theoretical. It’s daily. A missed dose. An extra pill. The wrong drug given because the labels look alike. These aren’t rare accidents. They’re systemic failures - and families need to know how to spot them and act.
What Counts as a Medication Mistake in Seniors?
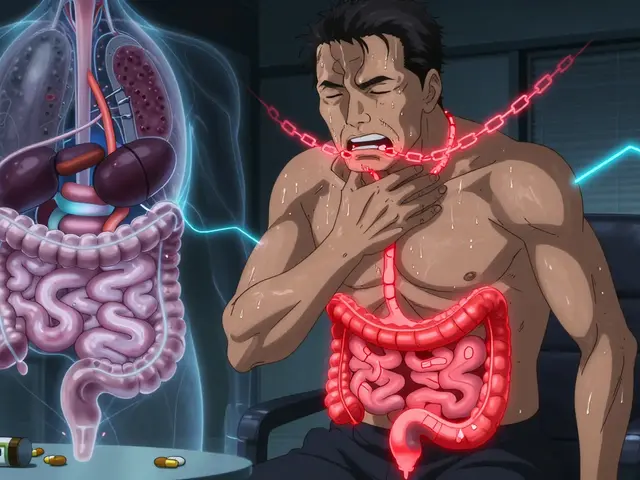
A medication error isn’t just when someone takes the wrong pill. It’s anything that leads to harm or the potential for harm because of how a drug is prescribed, given, or monitored. For older adults, the most common types include:- Wrong dosage - too much or too little, especially with drugs like blood thinners or diabetes medications
- Wrong time - giving medication at the wrong hour, like a nighttime sedative in the morning
- Wrong drug - mixing up similar-sounding names like hydrochlorothiazide and hydralazine
- Drug duplication - prescribing the same medicine under different brand names, like giving both Tylenol and a cold medicine that also contains acetaminophen
- Failure to monitor - not checking blood pressure, kidney function, or mental status after starting a new drug
- Expired or damaged meds - pills that are discolored, cracked, or past their expiration date still being given
- Documentation fraud - marking a medication as given when it never was
The Institute of Medicine found elderly patients suffer medication errors at three times the rate of younger adults. Why? Polypharmacy. Most seniors take five to ten prescriptions. Some take more than fifteen. Each additional drug increases the chance of interaction, confusion, or oversight.
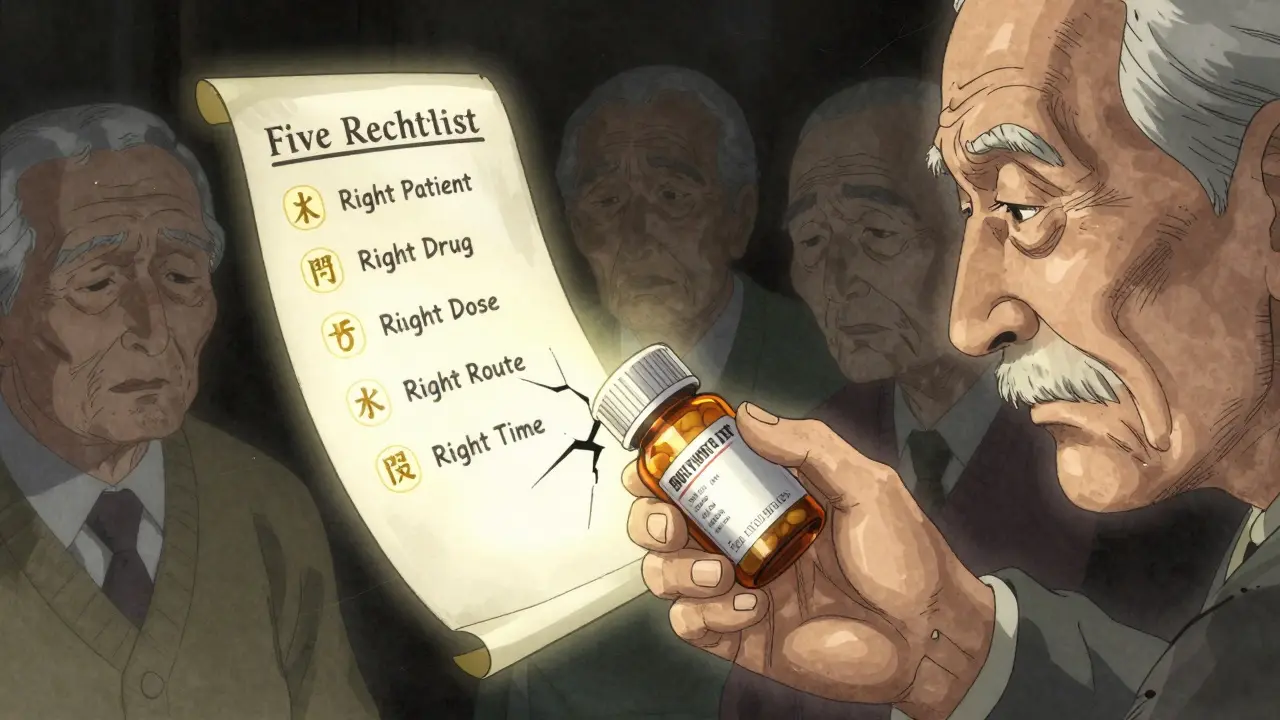
How to Spot a Medication Error - The Five Rights Checklist
You don’t need to be a nurse to catch a mistake. Start with the Five Rights every time a medication is given:- Right patient - Is this the correct person? Check the wristband or ID. Names can be similar.
- Right drug - Does the pill match the prescription? Look up the name and color online if unsure.
- Right dose - Is this the amount the doctor ordered? A 5mg tablet isn’t the same as a 10mg.
- Right route - Is it supposed to be swallowed, applied to the skin, or injected? Don’t assume.
- Right time - Is it being given at the scheduled hour? Morning meds shouldn’t be given at bedtime.
Studies show that following this checklist reduces errors by 63%. If even one item doesn’t match, stop. Ask. Double-check.
Also watch for signs your loved one is reacting badly:
- Sudden confusion or memory loss
- Unexplained bruising or bleeding
- Extreme drowsiness or agitation
- Loss of appetite or nausea without cause
- Falls or dizziness after a new drug is started
These aren’t just "getting older." They’re red flags.
Why Errors Keep Happening - And Why They’re Often Hidden
Most errors aren’t caused by evil staff. They’re caused by broken systems. Nursing homes are understaffed. The average is 2.1 nurses per 100 residents. That’s less than one nurse for every 50 people - including those needing help eating, bathing, and using the bathroom. When staff are overwhelmed, shortcuts happen.And when mistakes occur, facilities often cover them up. Family members on Reddit and in abuse case files report the same pattern: when they catch an error, staff say, "Your mom was confused," or "It was a one-time thing," or "We didn’t realize it was wrong."
One family in Seattle found their mother was getting double doses of blood pressure medication for three weeks. When they asked for an incident report, the administrator said, "We don’t document those unless it’s a death." That’s not just wrong - it’s illegal.
Many facilities fear lawsuits or fines, so they don’t report. But here’s the truth: voluntary reporting saves lives. The MEDMARX system, which lets staff report errors anonymously, has captured over 2 million errors since 1999. And 78% of facilities that use it make real changes within 90 days.
How to Report a Medication Error - Step by Step
If you suspect a mistake, don’t wait. Don’t hope it won’t happen again. Take action.- Document everything immediately - Write down the date, time, drug name, dose, who gave it, and what happened. Take photos of pill bottles if you can.
- Speak to the nurse or pharmacist on duty - Ask, "Can we review this medication record? I’m concerned about what happened." Stay calm but firm.
- Request a medication reconciliation - Ask for a full list of all medications, including over-the-counter and supplements. Compare it to what’s actually being given. The American Geriatrics Society’s Beers Criteria® lists 34 drugs that are dangerous for seniors - make sure none are on the list.
- Notify the prescribing doctor - Call the doctor who wrote the prescription. Tell them what happened. They may need to adjust the regimen.
- File a formal report - Every state has a Long-Term Care Ombudsman Program. Call 1-800-677-1116. They’re free, confidential, and legally required to investigate. In California, you must report within 24 hours for life-threatening errors. In Texas, you have 72 hours. Don’t wait.
- Report to the FDA - For serious adverse reactions (like hospitalization or death), file a report at www.fda.gov/medwatch (though links aren’t allowed, the name is fine).
Don’t be afraid to threaten to contact the state health department. One family in New York got their mother’s medication errors corrected after they said they’d file a complaint with the state - within 24 hours, the facility held a meeting and changed their entire medication protocol.
What Happens After You Report?
Once you report, the facility must investigate. They’ll review the incident, interview staff, and update records. In facilities using the AHRQ Common Formats system (used by 92% of hospitals), this process is standardized and tracked.But nursing homes lag behind. Only 48% use proper reporting systems. That’s why your report matters. It’s not just about your loved one - it’s about preventing the next mistake.
Some states now impose fines of $10,000 per unreported serious error. CMS’s new Five-Star Quality Rating System includes medication error rates as a key metric. Facilities that hide errors will lose ratings - and families will notice.
How Technology Is Helping - And Where It’s Falling Short
Hospitals are using computerized systems that cut errors by up to 55%. Barcode scanners ensure the right drug goes to the right person. Clinical decision tools warn doctors if a drug is risky for an elderly patient.But most nursing homes still use paper charts. Only 55% have barcode systems. Only 60% use electronic medication records (eMAR). The federal government required all nursing homes to have eMAR by the end of 2025 - but many aren’t ready.
AI tools like MedAware can now predict dangerous prescriptions with 94% accuracy. But they’re still rare in long-term care. Until these tools are widely adopted, families remain the last line of defense.
What You Can Do Right Now
You don’t need to wait for a crisis. Start today:- Keep a written list of every medication your loved one takes - including vitamins, supplements, and creams.
- Ask for a medication review with their doctor every 6 months.
- Visit often - at different times of day. Watch how meds are given.
- Ask staff to show you the medication log before each dose.
- Know the Beers Criteria®. If you see a drug like diazepam, chlorpheniramine, or indomethacin on the list, ask why it’s still being used.
- Join a local caregiver support group. Share what you learn.
Medication errors aren’t inevitable. They’re preventable. But they won’t stop unless someone speaks up. Your vigilance could save a life - maybe even your own parent’s.








yo i just checked my grandpa’s meds and turns out he’s been gettin’ tylenol AND that cold syrup with acetaminophen for months… no wonder he’s always zoned out. we’re gonna fix this tomorrow. thanks for the wake-up call.
so basically families are the only thing stopping nursing homes from killing old people with typos
let’s be real - this isn’t about errors. it’s about capitalism. 2.1 nurses per 100 residents? that’s not negligence, it’s profit optimization. you want change? defund the private equity firms running these places. not ‘check the wristband’ - burn the system down.
the pharmacokinetic burden on geriatric polypharmacy patients is exponentially compounded by non-compliant eMAR adoption rates and the absence of pharmacogenomic integration in long-term care protocols. we’re operating in a pre-21st century model while the science has moved to AI-driven precision therapeutics. the disconnect is not just systemic - it’s ethically indefensible.
While the Five Rights framework remains a foundational heuristic in medication safety, its efficacy is contingent upon the cognitive load of nursing staff, which, per Maslow’s hierarchy of needs, must first satisfy physiological and safety requirements before higher-order vigilance can be reliably enacted. The reduction of errors by 63% is statistically significant, yet it ignores the latent structural violence inherent in underfunded elder care infrastructure. One cannot expect compassion to emerge from exhaustion.
i’ve been doing this for 11 years - watching my mom get her meds from a home where the nurses were always rushing. i started taking photos of the pill bottles, writing down times, asking for the logbook before each dose. they thought i was overreacting. then one day, i caught them giving her a drug that was expired by 8 months. they tried to say it was ‘just a slip.’ i filed with the ombudsman. they changed the whole shift schedule. i didn’t do it for a medal. i did it because no one else would. you don’t have to be a nurse. you just have to care enough to look.
my dad’s facility says they’re ‘updating systems’ but they still hand-write everything. i brought them a tablet with barcode scanner app. they said ‘we don’t have training.’ i trained them myself. now they’re asking for more. sometimes the system breaks - but you don’t wait for it to fix itself. you become the fix.
This is not a call for vigilance - it is a condemnation of institutionalized elder abuse. The fact that families must act as de facto pharmacists and inspectors reveals a societal failure so profound it borders on criminal negligence. The 250,000 errors annually are not accidents. They are the measurable output of a system that treats human life as a line item. If you are reading this and you have a loved one in a nursing home - you are already complicit by silence. Act. Now. Before it’s too late.
you think this is bad? wait till you hear about the home where they gave morphine to a non-pain patient because the nurse was ‘too tired to read.’ and then they blamed the family for ‘not knowing the signs.’ if you’re not screaming about this, you’re part of the problem. i’ve filed 17 reports. i’ve seen them fire people. i’ve seen them change policies. it’s not hopeless - it’s just inconvenient for them.
my cousin in India says their elderly get care from family, not facilities. no meds mislabeled, no cover-ups. just love, attention, and a spoonful of honey with the pills. maybe we’re asking the wrong question - not how to fix the system, but why we let it break in the first place?
every time i see one of these posts i think - this is the american dream? old people getting forgotten because someone forgot to scan a barcode? we built rockets to mars but can’t get a pill bottle right? the fact that we accept this as normal is the real tragedy. i cried reading this. not because i’m weak - because we’re broken.
i don’t know how to say this without sounding dramatic… but i checked my grandma’s meds after reading this. she’s on a drug that’s on the beers criteria. i didn’t even know what that was. i called her doctor. they said ‘oh, we’ll review it.’ i’m not letting it go. i’m not being ‘overly emotional.’ i’m being her voice. and i’m not sorry.
Medication errors are not isolated incidents - they are symptoms of a civilization that has outsourced its moral responsibility to corporate entities and bureaucratic inertia. The fact that we require families to become forensic pharmacists to prevent harm reveals a profound erosion of communal care. We must not only reform systems - we must reimagine our relationship to aging, to vulnerability, and to the sacred duty of tending to those who once tended to us. This is not about policy. It is about the soul of a society.
if you’re not checking your parents’ meds, you’re a bad child. that’s it. no excuses. you think you’re busy? they’re dying. go look at the bottles. right now. i mean it.