Every time you grab a bottle of pain relievers, cold medicine, or antacid off the shelf, you’re holding a product designed to help you feel better. But do you actually know what’s inside it? Most people don’t. And that’s where the real risk lies.
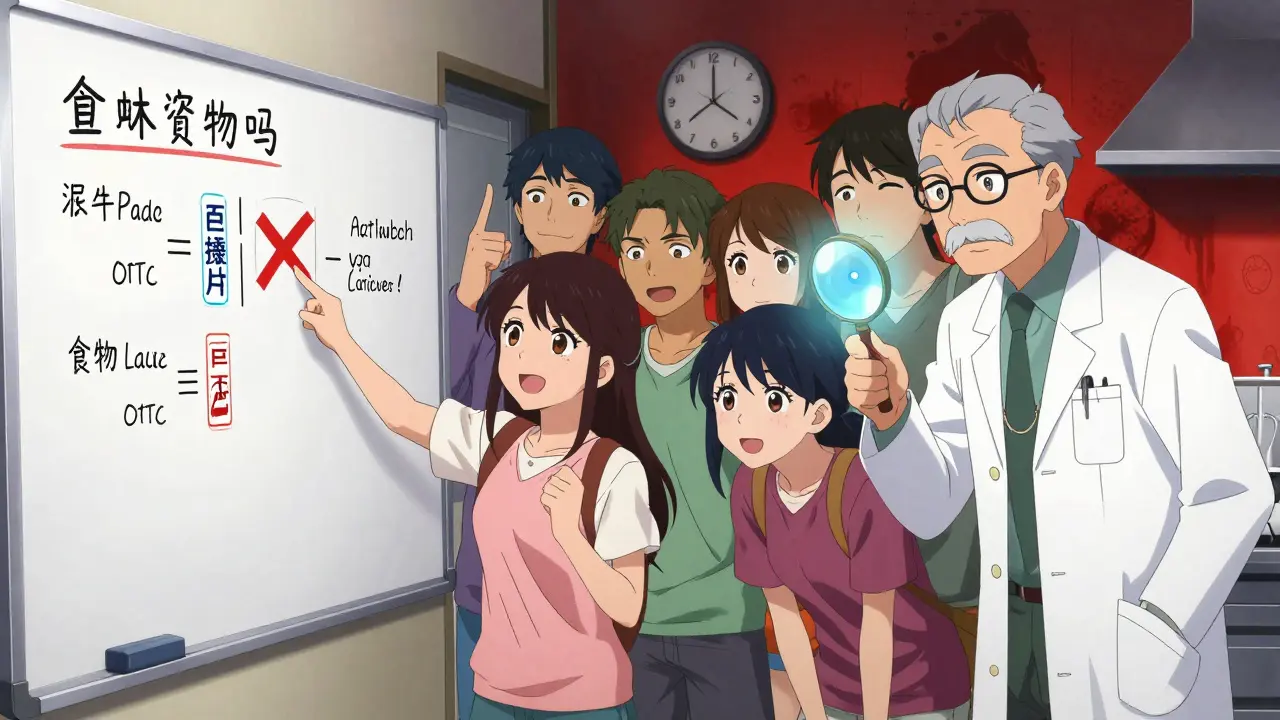
What Exactly Is an Active Ingredient?
The active ingredient is the part of the medicine that actually does the work. It’s the chemical that reduces fever, blocks allergies, or eases pain. Everything else - the colors, flavors, fillers, and coatings - is there to make the pill easier to swallow or look nice. But only the active ingredient changes how your body feels.
In the U.S., the FDA requires every over-the-counter (OTC) drug to list its active ingredients clearly on the Drug Facts label. This label isn’t optional. It’s the law. And it’s the only reliable way to know what you’re taking.
Take acetaminophen, for example. You’ll find it in Tylenol, Excedrin, TheraFlu, and even some prescription painkillers. It’s the same chemical no matter the brand. But if you take two different products that both contain acetaminophen - say, Tylenol for your headache and a nighttime cold medicine for your stuffy nose - you could accidentally double your dose. And that can damage your liver.
How to Read the Drug Facts Label
The Drug Facts label has seven sections, and the first one is the most important: Active Ingredients. This section lists every active compound in the product, in order of amount, with exact milligram or percentage amounts. Here’s what it looks like on a typical multi-symptom cold tablet:
- Acetaminophen 325 mg
- Dextromethorphan hydrobromide 15 mg
- Phenylephrine hydrochloride 5 mg
Each line tells you exactly what chemical is doing what. Acetaminophen reduces pain and fever. Dextromethorphan suppresses coughs. Phenylephrine shrinks swollen nasal passages. If you’re on blood pressure meds, phenylephrine could raise your numbers. If you drink alcohol, acetaminophen becomes more dangerous. You won’t know any of this unless you read the label.
The FDA doesn’t allow vague terms like “natural pain relief” or “proprietary blend.” Every active ingredient must be named by its official United States Adopted Name (USAN). That means “ibuprofen,” not “pain reliever formula.” And the amount? It has to be precise - within 10% of what’s printed. No guessing.
Why Brand Names Are Misleading
When you see “Advil,” “Motrin,” or “Nuprin,” you might think they’re different medicines. They’re not. They all contain ibuprofen. Same with “Aleve” - that’s naproxen sodium. And “Benadryl”? That’s diphenhydramine. The brand name is just marketing. The active ingredient is what matters.
A 2023 Consumer Reports survey found that only 28% of adults could correctly identify that Aleve contains naproxen sodium. Meanwhile, 72% knew Tylenol contains acetaminophen. Why the gap? Because Tylenol is so widely known. But that’s not enough. If you don’t know what’s in your cold medicine, you might take it with Tylenol - and end up with 1,000 mg of acetaminophen in one dose. That’s twice the safe limit for some people.
Even more alarming: a Reddit thread from 2022 shared stories of people ending up in the ER after combining cold meds with Tylenol. One user took TheraFlu Nighttime thinking it was just a sleep aid. Didn’t realize it had 650 mg of acetaminophen. They’d already taken two Tylenol tablets earlier. Total dose? 1,300 mg - enough to cause liver toxicity. That’s preventable.
Common Active Ingredients You Should Know
You don’t need to memorize all 800+ active ingredients in OTC drugs. But these 10 cover 70% of what you’ll see on shelves:
- Acetaminophen - Pain and fever relief. Max daily dose: 4,000 mg for adults. Found in over 600 products.
- Ibuprofen - Anti-inflammatory pain relief. Max dose: 1,200 mg/day for OTC. Found in Advil, Motrin.
- Naproxen sodium - Longer-lasting pain relief. Found in Aleve. Max dose: 660 mg/day.
- Diphenhydramine - Allergy and sleep aid. Found in Benadryl, NyQuil. Max dose: 50 mg per dose.
- Cetirizine - Non-drowsy allergy relief. Found in Zyrtec. Max dose: 10 mg/day.
- Pseudoephedrine - Nasal decongestant. Found in Sudafed. Requires ID to buy.
- Phenylephrine - Alternative decongestant. Less effective than pseudoephedrine. Found in many cold meds.
- Dextromethorphan - Cough suppressant. Found in Robitussin, DayQuil. Abuse risk if taken in large doses.
- Loperamide - Anti-diarrheal. Found in Imodium. Misuse can cause heart problems - 162 deaths reported between 2012-2022.
- Calcium carbonate - Antacid. Found in Tums. Also used as a calcium supplement.
Notice how some ingredients serve multiple purposes? Diphenhydramine helps with allergies and sleep. Acetaminophen is in pain relievers, cold meds, and sleep aids. That’s why checking the label every single time is non-negotiable.
The Hidden Danger: Duplicate Ingredients
Most medication errors happen because people take more than one product without realizing they contain the same active ingredient.
A 2023 study by the American Society of Health-System Pharmacists showed that using a simple “Active Ingredient Cross-Check” - writing down every active ingredient from each product you buy - prevented 82% of potential acetaminophen overdoses in a test group of 500 shoppers.
Here’s how to do it:
- Before buying anything, write down the active ingredients from any medicine you’re already taking.
- When you pick up a new OTC product, read the Drug Facts label and add those ingredients to your list.
- Look for duplicates. If you see acetaminophen on both lists, don’t take them together.
- If you’re unsure, ask a pharmacist. They’re trained to catch these overlaps.
It takes 45 seconds. That’s all it takes to avoid a trip to the ER.
What About Children’s Medicines?
Parents are especially vulnerable to confusion. Children’s Motrin and Children’s Zyrtec look similar - both come in liquid form, both have bright packaging. But one has ibuprofen. The other has cetirizine. One treats fever and pain. The other treats allergies. Give the wrong one, and you’re not helping - you’re risking side effects.
Nationwide Children’s Hospital recommends parents always check the active ingredient, not the brand name. Their study showed that parents who spent at least 45 seconds reading the label reduced medication errors by 68%.
And don’t assume “children’s” means safer. Children’s Tylenol still contains acetaminophen. The dose is lower, but if you give too much - or combine it with another product - the risk is the same.
What’s Changing in 2026?
The FDA is pushing for digital labels. By 2026, most OTC drugs will include a QR code that links to a full digital Drug Facts label. This isn’t just for convenience. It’s because many people - especially older adults and those with low health literacy - can’t read small print.
Early tests showed that when people scanned the QR code, their understanding of active ingredients improved by 47%. The new labels will also include clearer warnings about inactive ingredients - like red dye #40, which can trigger allergic reactions in sensitive kids.
But here’s the catch: the QR code doesn’t replace the printed label. You still need to read the printed one. The digital version is a backup, not a shortcut.
What to Do Next
You don’t need to be a pharmacist to use OTC drugs safely. You just need to be careful.
Here’s your simple action plan:
- Always read the Drug Facts label - even if you’ve bought the product before. Ingredients change.
- Write down the active ingredients in every medicine you take, including vitamins and supplements.
- Never combine two products with the same active ingredient unless a doctor says it’s safe.
- If you’re pregnant, have liver disease, or take blood thinners, check with a pharmacist before using any OTC drug.
- Download the FDA’s free Active Ingredient Reference Chart. It lists 35 common ingredients with their uses and max doses.
OTC drugs are powerful. They’re not candy. They’re not harmless. They’re medicine - and medicine, even when it’s sold on a shelf, can hurt you if you don’t know what you’re taking.
Next time you reach for a bottle, pause. Look at the label. Know what’s inside. Your body will thank you.
How do I know if two OTC medicines have the same active ingredient?
Always check the "Active Ingredients" section on the Drug Facts label. Even if the brand names are different - like Tylenol and a store-brand pain reliever - they may both contain acetaminophen. Write down each active ingredient from every product you’re using. If any names match, you’re doubling up. Avoid combining them.
Can I take OTC medicine if I’m on prescription drugs?
Not always. Many OTC drugs interact with prescription medications. For example, ibuprofen can increase bleeding risk if you’re on blood thinners. Pseudoephedrine can raise blood pressure if you have hypertension. Always check with your pharmacist before mixing OTC and prescription drugs - even if they seem harmless.
Why do some OTC drugs have lower doses than prescription versions?
The FDA limits OTC doses to ensure safety for self-use. For example, prescription ibuprofen can be 600-800 mg per tablet, while OTC is capped at 200 mg. This reduces the risk of overdose, stomach bleeding, or kidney damage when people don’t have medical supervision. Higher doses require a doctor’s guidance.
Are generic OTC brands as safe as name brands?
Yes. Generic OTC drugs must contain the same active ingredient, in the same amount, and work the same way as the brand name. The FDA requires them to meet the same standards. The only differences are in inactive ingredients (like color or flavor) and price. Always check the active ingredient list - that’s what matters.
What should I do if I accidentally take too much of an OTC drug?
Call Poison Control immediately at 1-800-222-1222. Don’t wait for symptoms. For acetaminophen overdose, liver damage can start within hours. For ibuprofen, stomach bleeding or kidney issues can follow. Keep the medicine bottle handy - the poison control center will ask for the active ingredient and how much you took.
Is it safe to use expired OTC medicine?
Most OTC drugs lose effectiveness over time, but few become dangerous. However, for critical meds like epinephrine auto-injectors or antibiotics, never use expired ones. For pain relievers or antacids, if they’re just a few months past the date and look normal, they’re likely still safe. But don’t rely on them for serious symptoms. Replace them.
Why do some OTC labels say "contains acetaminophen" while others don’t?
All FDA-approved OTC products must list active ingredients on the Drug Facts label. If you don’t see it, the product may be unregulated, counterfeit, or sold illegally. Be cautious of products sold online or in convenience stores without a Drug Facts label. Legitimate OTC drugs always have one.









Most people treat OTC meds like candy-grab one, toss it back, no questions asked. Then they wonder why they feel like a ghost after a weekend of ‘just one more’ cold pills. The Drug Facts label isn’t decoration. It’s your last line of defense against accidental self-poisoning. I’ve seen guys stack NyQuil, Tylenol, and ‘energy boosters’ like they’re playing Jenga with their liver. Don’t be that guy.
Reading labels feels like decoding ancient runes sometimes-until you realize it’s just plain English. Acetaminophen? That’s Tylenol. Ibuprofen? Advil. Naproxen? Aleve. They’re not magic spells. They’re chemicals. And if you’re taking two things with the same chemical, you’re not being smart-you’re being lazy. I keep a little notepad on my fridge now. Active ingredients only. Saves lives. And sanity.
In India, we call this ‘dawa ka naam’-the name of the medicine. But everyone just asks for ‘painkiller’ or ‘cold relief.’ No one checks the chemical. My aunt once took a cough syrup with dextromethorphan and her sleeping pill with diphenhydramine-both are sedatives. She slept for 18 hours straight. Woke up confused, scared, but alive. That’s the kind of story that sticks with you. Read the label. Even if you think you know what you’re doing.
Guys, I used to think OTC meant ‘Oh, That’s Cool’-like, it’s just medicine you can buy without a prescription, so it must be safe, right? Wrong. So wrong. I once took a cold med with acetaminophen and then grabbed a Tylenol for a headache because I ‘just needed a little more.’ Didn’t realize I’d hit 3,000 mg in under 4 hours. Felt like my insides were being slowly dissolved. Ended up in urgent care. They said I got lucky. Now I have a sticky note on my medicine cabinet that says: ‘ONE ACTIVE INGREDIENT AT A TIME.’ It’s not a suggestion. It’s a survival rule. And if you’re a parent? Same rule. Kids’ meds aren’t toys. They’re potent. Treat them like dynamite-because that’s what they are if you misread the label.
I used to think generics were ‘cheap versions’ of real medicine-until I learned they’re literally the same chemical, same dose, same effect. I switched to store-brand ibuprofen and saved $15 a bottle. No difference in how my knee felt. The only thing different? The color of the pill. And the price. So next time you’re tempted to buy the fancy bottle with the cool logo, just flip it over and check the active ingredient. If it’s ibuprofen, you’re golden. No need to pay extra for marketing.
People don’t understand dosage. They think more is better. They think if one pill helps, two will help more. They think the body is a machine that runs on volume. It’s not. It’s a fragile ecosystem. And acetaminophen? It’s a silent killer. No screaming. No warning. Just enzymes dying one by one. And no one notices until it’s too late. The FDA limits OTC doses because they know how dumb humans are. And they’re right.
The erosion of personal responsibility in American healthcare is staggering. We have a nation that demands transparency in product labeling, yet refuses to read it. We have a culture that glorifies convenience over competence. The Drug Facts label is not a suggestion. It is a civic duty. To ignore it is not ignorance-it is moral negligence. The FDA has done its part. Now it is up to the individual to exercise intellectual discipline. Will you rise to the occasion, or will you remain another statistic in the graveyard of self-inflicted harm?
Just read the damn label. 🙄
Acetaminophen + NyQuil = bad time.
Ibuprofen + blood thinner = ER party.
Diphenhydramine + alcohol = you won’t remember your own name.
It’s not rocket science. It’s not even high school chemistry. It’s reading. You can do it. Stop being lazy. Your liver is begging you.
Pharmacokinetic interactions are often underappreciated in the OTC space. The hepatic metabolism of acetaminophen via CYP2E1 and CYP3A4 is particularly vulnerable to enzyme induction from ethanol or concurrent use of anticonvulsants. Phenylephrine’s alpha-1 agonism may exacerbate hypertension in patients on MAOIs or beta-blockers. The lack of standardized patient education infrastructure exacerbates polypharmacy risks. QR codes are a step, but real change requires embedded clinical decision support at point-of-sale.
I get it. Labels are small. It’s confusing. I used to skip them too-until my mom had a bad reaction to a cold med because it had pseudoephedrine and she had high blood pressure. She’s fine now, but I’ll never skip reading again. I started writing down every active ingredient in a little notebook. I even showed my dad how to do it. He’s 72. He says it feels like learning to drive again. But he says it’s worth it. Maybe we don’t need fancy apps. Maybe we just need to slow down. And read.
Why do you care so much? Just take the pill. It’s not like you’re gonna die. Everyone does it. You’re overthinking. Chill out. It’s just medicine. What’s the worst that could happen?