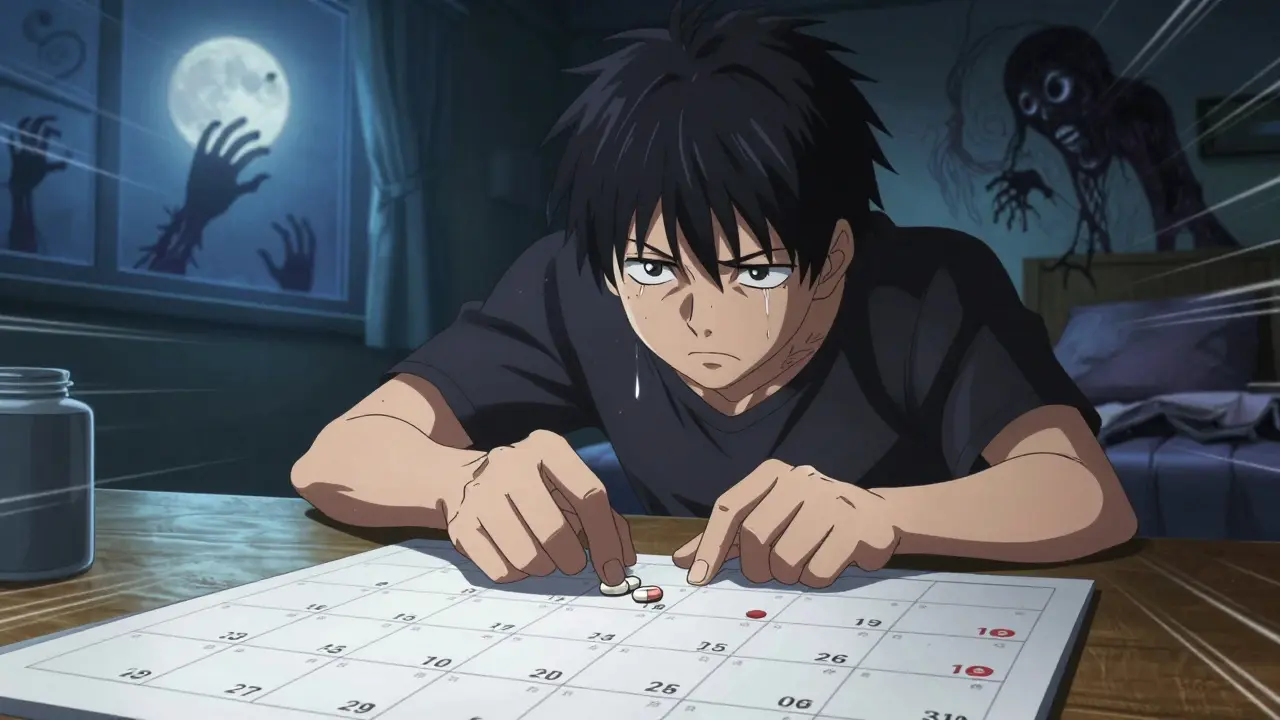
Stopping benzodiazepines cold turkey can be dangerous. For people who’ve been taking them for months or years-whether for anxiety, insomnia, or muscle spasms-sudden withdrawal can trigger seizures, panic attacks, hallucinations, or even life-threatening complications. The good news? You don’t have to quit all at once. A benzodiazepine tapering plan, done slowly and with support, can help you reduce dependence safely and regain control of your life.
Why Tapering Is Necessary
Benzodiazepines like Xanax, Valium, and Klonopin work quickly to calm the nervous system. That’s why they’re so effective for short-term use. But after about four to six weeks of daily use, your brain starts to adapt. It begins relying on the drug to maintain balance. When you stop, your brain is left without its chemical crutch-and that’s when withdrawal kicks in. The 2024 Joint Clinical Practice Guideline, backed by 10 major medical societies, confirms that tapering is the only safe way to stop long-term benzodiazepine use. Abrupt discontinuation carries a 20-40% risk of severe withdrawal, especially with short-acting drugs like alprazolam. Symptoms can include intense anxiety, insomnia, tremors, muscle pain, nausea, and even seizures. For older adults, the risks are even higher: falls, confusion, and car accidents increase significantly.How Slow Should a Taper Be?
There’s no universal timeline. Your taper speed depends on how long you’ve been taking the medication, your dose, your health, and your personal tolerance for symptoms. The 2024 guidelines recommend starting with a 5-10% reduction in your total daily dose every 2-4 weeks. This is the sweet spot for most people: slow enough to avoid severe symptoms, fast enough to prevent getting stuck in the process. Here’s a general breakdown based on duration of use:- 2-8 weeks of use: Taper over at least 2 weeks
- 8 weeks to 6 months: Taper over at least 4 weeks
- 6 months to 1 year: Taper over at least 8 weeks
- Over 1 year: Taper over 6-18 months
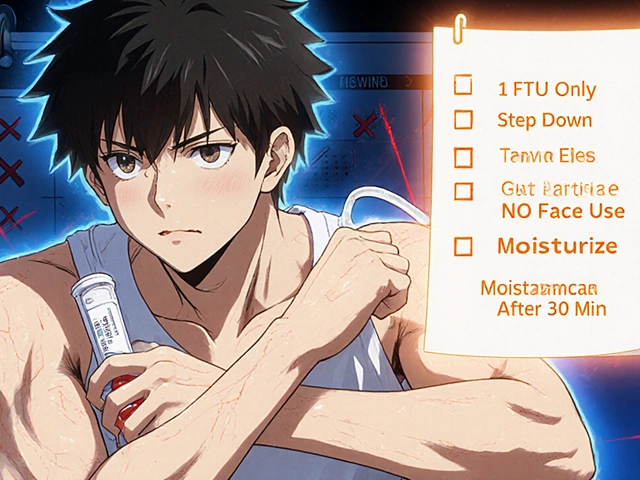
Choosing the Right Tapering Method
There are three main approaches to tapering, each with pros and cons. 1. Stay on the same medication - If you’re on a longer-acting benzo like diazepam (Valium), you can often taper directly. Diazepam has a long half-life, meaning it stays in your system longer, which smooths out withdrawal symptoms. It’s often the preferred choice for tapering. 2. Switch to a longer-acting benzo - If you’re on a short-acting drug like alprazolam (Xanax), switching to diazepam can make the process easier. The conversion isn’t one-to-one: 1 mg of alprazolam equals about 20 mg of diazepam. Your doctor will use a conversion table to match your current dose to an equivalent dose of diazepam, then taper from there. 3. Use adjunctive medications - Sometimes, doctors add other medications to help manage withdrawal symptoms. This might include antidepressants like SSRIs for anxiety, sleep aids like trazodone for insomnia, or beta-blockers for heart palpitations. These aren’t replacements for tapering-they’re support tools.Who Should Taper?
Not everyone needs to stop. But for many, the risks of long-term use outweigh the benefits. The guidelines recommend tapering for:- Older adults (65+), due to increased risk of falls and cognitive decline
- People taking multiple benzodiazepines or combining them with opioids or stimulants
- Those with a history of substance use disorder
- Patients with traumatic brain injury or dementia
- People with PTSD, especially veterans-benzodiazepines can interfere with trauma-focused therapy

What to Expect During Tapering
Withdrawal symptoms don’t always show up right away. Sometimes, they creep in days after a dose reduction. Common signs include:- Increased anxiety or panic
- Difficulty sleeping
- Headaches or dizziness
- Tingling or numbness in hands and feet
- Light and sound sensitivity
- Heart palpitations
- Nausea or digestive issues
Support Is Critical
Tapering isn’t just a medical process. It’s emotional. Many people feel isolated, scared, or guilty about needing help. That’s why support makes all the difference. The VA and other leading programs now include peer support specialists-people who’ve successfully tapered themselves-in their treatment teams. These individuals offer real-life advice, encouragement, and accountability. Studies show that when CBT is combined with tapering, success rates jump from 42% to nearly 68%. You also need consistent check-ins with your prescriber. Weekly or biweekly visits are ideal, especially early in the taper. Your doctor should track your symptoms, adjust your schedule as needed, and help you build new coping skills-like breathing exercises, mindfulness, or daily movement-to replace the calming effect the drug once provided.What to Avoid
Some common mistakes make tapering harder-or dangerous.- Self-tapering without medical supervision - Even if you feel fine, withdrawal can sneak up on you. A doctor can catch early signs of complications.
- Switching between different benzos - This confuses your body and increases withdrawal risk. Stick to one medication during the taper.
- Using alcohol or other sedatives - This masks symptoms but increases overdose risk and delays true recovery.
- Waiting until you’re in crisis to start - If you’re already having panic attacks or insomnia, it’s harder to taper. Plan ahead.

Real-World Progress
Since 2020, the Department of Veterans Affairs has mandated tapering for high-risk veterans. The result? A 23.7% drop in long-term benzodiazepine prescriptions in just three years. In states like Oregon and Washington, laws now require tapering plans for prescriptions lasting more than 90 days. Meanwhile, new tools are emerging. The NIH is funding a mobile app that tracks symptoms in real time and suggests dose adjustments based on your input. It’s set to launch in 2026, offering a new level of personalized support.When Tapering Isn’t the Answer
Some people need to stay on low-dose benzodiazepines long-term. If you’ve tried everything-therapy, other meds, lifestyle changes-and your anxiety or insomnia is still unmanageable, staying on a minimal dose might be the safest option. The goal isn’t to stop at all costs. It’s to reduce harm and improve quality of life. If you’re on a low dose, feeling stable, and not experiencing side effects, your doctor may decide to maintain your current regimen. That’s not failure. It’s informed care.Next Steps
If you’re considering tapering:- Don’t change your dose on your own. Talk to your prescriber.
- Ask for a copy of your medication history and current dose.
- Request a taper plan that includes check-ins every 2-4 weeks.
- Ask about CBT or counseling to support the process.
- Use one pharmacy and one doctor to avoid accidental overuse.
- Track your symptoms daily-even small changes matter.
Can I taper off benzodiazepines on my own?
No. Tapering without medical supervision increases the risk of severe withdrawal, including seizures. Even if you feel fine, your body may be adapting in ways you can’t detect. A doctor can monitor your symptoms, adjust your schedule, and intervene if complications arise. Never stop or reduce your dose without professional guidance.
How long does it take to fully taper off benzos?
It varies. For short-term users (under 6 months), it can take 4-8 weeks. For long-term users (over a year), it often takes 6-18 months. Some people need up to two years, especially if they’ve been on high doses or have a history of anxiety disorders. The key is going slow enough to avoid severe symptoms, not fast enough to meet a deadline.
Is diazepam (Valium) better than Xanax for tapering?
Yes, for most people. Diazepam has a long half-life (20-100 hours), which means it stays in your system longer and provides a smoother decline in drug levels. Alprazolam (Xanax) has a short half-life (6-12 hours), causing sharp drops in blood concentration that trigger withdrawal symptoms. Switching from Xanax to diazepam before tapering is a common and safer strategy.
Will I feel better after tapering?
Most people do-but not right away. Withdrawal symptoms can last weeks or months. But once your brain readjusts, many report improved sleep, clearer thinking, less brain fog, and better emotional regulation. Studies show that people who successfully taper often feel more in control of their lives and less dependent on medication.
What if my anxiety comes back during tapering?
It’s common. Anxiety often returns as your body adjusts. The goal isn’t to eliminate anxiety completely-it’s to manage it without drugs. Work with a therapist trained in CBT to learn coping tools like breathing techniques, exposure therapy, and mindfulness. These skills are more effective long-term than any medication.
Are there any new treatments for benzodiazepine withdrawal?
Yes. A new NIH-funded mobile app, expected in 2026, will help track symptoms and suggest personalized taper adjustments. Some clinics now offer ketamine-assisted therapy for severe withdrawal, though it’s still experimental. The most proven approach remains a slow taper combined with cognitive behavioral therapy and peer support.







This post is fire. I tapered off Xanax after 5 years and it nearly killed me-but I did it. No doctor, no support, just grit and a dumbass notebook tracking every panic attack. I lost 15 pounds. Couldn’t sleep for 87 days straight. But now? I’m clearer than I’ve been since college. If you’re scared, good. That means you’re alive. Don’t quit. Just go slower.
Bro, this ain’t just medical-it’s spiritual. Benzodiazepines are like emotional handcuffs. You think you’re calm, but you’re just numbed. Tapering? It’s the ultimate act of reclaiming your soul. I switched from alprazolam to diazepam like swapping a firecracker for a candle. Slow burn, baby. And when the nights got dark? I danced in my living room to old Bollywood tunes. Turned panic into poetry. You got this.
Stop romanticizing tapering. It’s not a journey. It’s a clinical process with documented protocols. You don’t dance to Bollywood during withdrawal. You follow the 2024 Joint Guideline: 5-10% every 2-4 weeks. Diazepam conversion ratios are non-negotiable. 1mg alprazolam = 20mg diazepam. Not 15. Not 25. 20. If you’re using ‘mindfulness’ as a substitute for medical supervision you’re endangering yourself. Also stop posting about ‘feeling clearer.’ That’s anecdotal nonsense. Track your GAD-7 scores.
Thank you for this. I’ve been tapering for 11 months and I still have days where I feel like I’m underwater. But I’m still here. I started at 4mg of Klonopin. Now I’m at 0.3mg. I cried in the grocery store last week because I forgot to buy milk. That’s okay. Progress isn’t linear. I found a therapist who doesn’t rush me. I walk 20 minutes every morning. I don’t always feel better. But I feel more like me. That’s enough.
omg i just started my taper last week and i was so scared but this post made me feel less alone. i switched to valium and my hands stopped shaking kinda. still cant sleep but i’m drinking chamomile tea and listening to rain sounds. it’s gonna be a long road but i’m trying. thank you for writing this ❤️
People who taper without supervision are irresponsible. You’re not a hero. You’re a statistic waiting to happen. Seizures don’t care about your ‘journey.’ If you’re using Reddit as your primary care provider, you’re doing it wrong. The VA doesn’t do ‘tough love.’ They do protocols. Follow them. Or don’t. But don’t pretend your Instagram wellness vibe is medicine.
There’s a quiet dignity in the slow unraveling of dependence. We’ve been taught to fix things fast-to crush the problem, not sit with it. But the nervous system doesn’t negotiate. It remembers. Every milligram you remove is a whisper to your brain: ‘You’re safe without this.’ The anxiety returns? Good. It’s not your enemy. It’s your teacher. Sit with it. Breathe. Let it pass. You’re not broken. You’re becoming.
I read all the comments. I’m 6 months in. Still on 0.5mg diazepam. Had a panic attack yesterday. Called my peer support specialist. She didn’t fix it. She just said ‘I’ve been there. You’re not alone.’ That’s all I needed. If you’re reading this and scared-reach out. Even just to say ‘I’m still here.’ That’s enough. You’re doing better than you think.