CBD Drug Interaction Checker
Your Medications
Select all medications you're currently taking
Interaction Results
Based on CYP450 enzyme inhibition
Millions of Americans use CBD oil for sleep, pain, or anxiety-but what happens when it meets your prescription meds? If you're taking blood thinners, antidepressants, seizure drugs, or even painkillers, mixing them with CBD could be riskier than you think. It’s not just about feeling drowsy. There’s a hidden mechanism in your liver that’s silently changing how your body handles your medications-and it’s called CYP450 inhibition.
How CBD Changes the Way Your Body Processes Medications
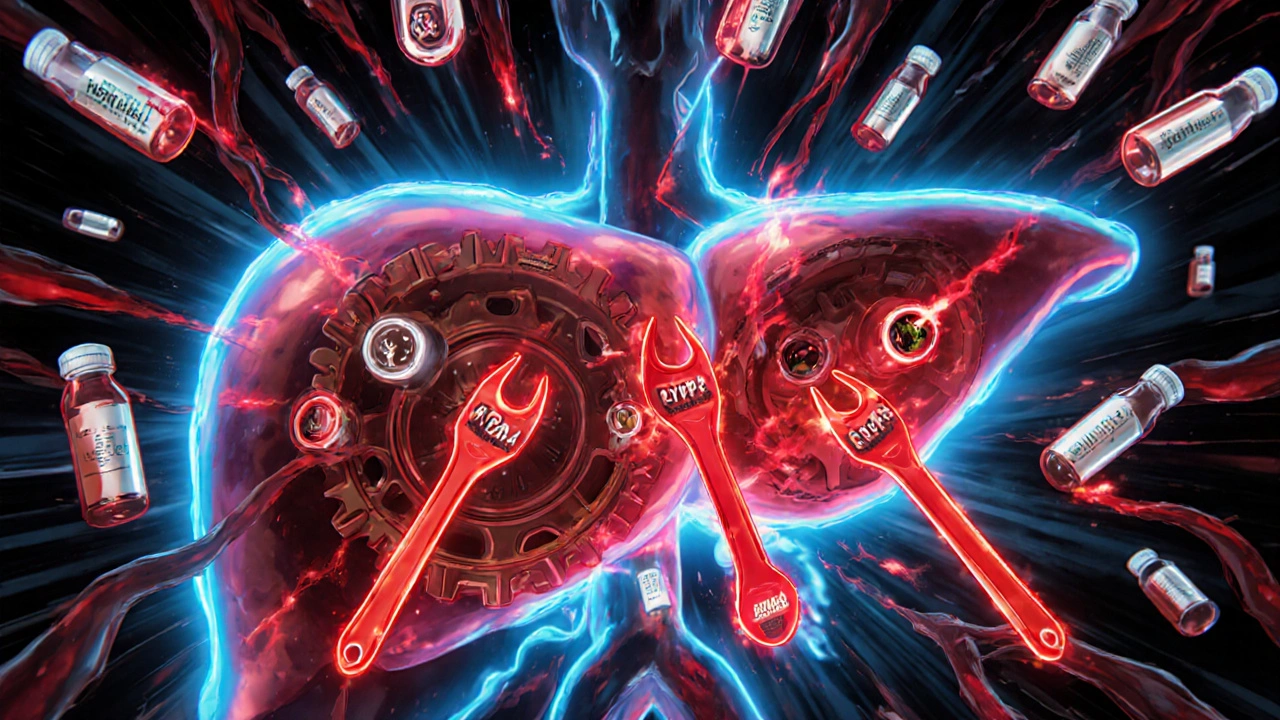
Your liver uses a family of enzymes called cytochrome P450 (CYP450) to break down about 70-80% of all prescription drugs. These enzymes act like molecular scissors, cutting up medications so your body can get rid of them. But CBD doesn’t just pass through-it steps in and blocks these enzymes. Think of it like jamming a wrench into a machine that’s supposed to be running smoothly. The most affected enzymes are CYP2C9, CYP2C19, CYP3A4, and CYP2D6. These handle common drugs like warfarin (a blood thinner), clobazam (an anti-seizure medicine), sertraline (an antidepressant), and fentanyl (a painkiller). When CBD blocks them, your meds don’t get broken down as fast. That means they build up in your bloodstream. Higher levels = stronger effects. And sometimes, those effects are dangerous. For example, if you’re on warfarin and start taking CBD, your INR (a measure of blood clotting) can spike from a safe 2.5 to a dangerous 5.8. That’s what happened to one patient who ended up in the ER needing vitamin K to reverse the risk of internal bleeding. This isn’t rare. The FDA’s adverse event database has over 140 reports of sedation or bleeding linked to CBD and prescription drugs between 2018 and 2023.Why Sedation Happens-And Why It’s Not Just ‘Feeling Relaxed’
Many people assume that feeling sleepy after taking CBD is just the calming effect they wanted. But sometimes, it’s not CBD at all. It’s your other meds piling up because CBD shut down their breakdown pathway. Take clobazam, a common drug for epilepsy. When taken with Epidiolex (a purified CBD medication), the active metabolite of clobazam, called N-desmethylclobazam, can increase by 60%. That’s not a small bump-it’s a clinical surge. One patient on Reddit reported going from 600 ng/mL to 1,050 ng/mL of that metabolite in just two weeks. The result? Extreme drowsiness, confusion, and falls. Her neurologist had to cut her clobazam dose in half. Same thing happens with benzodiazepines like lorazepam or alprazolam. CBD doesn’t just make you sleepy-it keeps your existing sedatives in your system longer. Combine that with sleep aids like zolpidem or even alcohol, and you’re stacking up CNS depressants. The risk? Respiratory depression, loss of coordination, or worse. A 2023 study of 217 medical cannabis users found that 34% experienced increased sedation when combining CBD with their prescriptions. For those on CYP2C19-metabolized drugs, the rate jumped to 58%. That’s more than half.Which Medications Are Most at Risk?
Not all drugs are equally affected. Some are like ticking time bombs when mixed with CBD. Here’s who’s most at risk:- Warfarin (CYP2C9): Risk of dangerous bleeding. INR levels can spike unpredictably.
- Clobazam, Valproate (CYP2C19): Seizure meds that can cause toxic buildup and sedation.
- SSRIs and SNRIs like sertraline, fluoxetine, venlafaxine (CYP2D6): Increased risk of serotonin syndrome, dizziness, or heart rhythm issues.
- Fentanyl, Oxycodone (CYP3A4): Slower metabolism means prolonged pain relief-but also higher overdose risk.
- Statins like atorvastatin (CYP3A4): Increased chance of muscle damage (rhabdomyolysis).
- Calcium channel blockers like amlodipine (CYP3A4): Can cause low blood pressure or dizziness.

Real-World Cases: When CBD Goes Wrong
Patient stories aren’t just anecdotes-they’re warning signs. One man in Ohio started taking a 25 mg CBD tincture for back pain. He was already on metoprolol (a beta-blocker) and sertraline. Within a week, he felt dizzy, nauseous, and his heart rate dropped to 48 bpm. His doctor pulled his bloodwork: sertraline levels were 3x higher than normal. He stopped CBD. Symptoms cleared in 48 hours. Another woman in Florida took CBD for anxiety and was on levothyroxine for hypothyroidism. Her TSH levels jumped from 2.1 to 7.8-suggesting her thyroid meds weren’t being absorbed properly. Her pharmacist flagged it: CBD can interfere with thyroid hormone transporters, not just CYP enzymes. Even people who think they’re being careful get caught. One user on Healthgrades said she used CBD to reduce her fentanyl dose by 40%. Her doctor approved it, thinking the inhibition would help. But she didn’t realize the effect could last days after stopping CBD. When she skipped a dose, her pain returned harder than before-because her body had adapted to higher fentanyl levels.What You Can Do: Safe Practices and Solutions
You don’t have to quit CBD if you’re on meds. But you need a plan.- Know your meds. Check if your prescriptions are metabolized by CYP2C9, CYP2C19, CYP3A4, or CYP2D6. Ask your pharmacist or use the free Drug Interaction Checker from the University of Washington (coming June 2024).
- Start low and go slow. If you’re new to CBD, begin with 5-10 mg per day. Wait at least 7 days before increasing. Monitor for drowsiness, dizziness, or unusual side effects.
- Time your doses. Separate CBD and your meds by 2-4 hours. This doesn’t stop inhibition, but it reduces peak overlap.
- Get blood tests. If you’re on warfarin, clobazam, or other narrow-therapeutic-index drugs, ask for a blood level check 3-5 days after starting CBD.
- Don’t trust labels. Buy CBD from companies that provide third-party Certificates of Analysis (COAs). Look for testing for potency and contaminants.
- Consider alternatives. CBG and CBC show less CYP inhibition in early studies. They’re not magic bullets, but they might be safer options if you need cannabinoids without the interaction risk.

The Bigger Picture: Regulation, Research, and the Future
The CBD market hit $28.6 billion in 2023. Yet, the FDA still hasn’t set standards for purity, labeling, or safety warnings. In 2023, they sent warning letters to 15 companies for failing to mention drug interactions on their labels. Meanwhile, science is catching up. The NIH is running a major trial (NCT04893224) testing CBD’s effect on warfarin in 120 people. Results are expected by late 2024. The European Medicines Agency now requires all cannabinoid drugs to include CYP450 interaction data-something the U.S. still doesn’t enforce for over-the-counter products. Pharmacists are finally being trained. In 2024, the American Pharmacists Association made 3 hours of cannabinoid-drug interaction education mandatory for license renewal. More than 1,200 clinicians have already completed the University of Maryland’s CME course on this topic. The future may hold smarter CBD products-like nanoparticle formulations that avoid liver metabolism entirely. But until then, the safest approach is simple: talk to your doctor before mixing CBD with anything you take by prescription.Frequently Asked Questions
Can I take CBD with my blood pressure medication?
It depends. CBD can interact with calcium channel blockers like amlodipine and beta-blockers like metoprolol because they’re processed by CYP3A4 and CYP2D6. This can cause your blood pressure to drop too low, leading to dizziness or fainting. If you’re on these meds, start with a very low CBD dose (5 mg or less), monitor your blood pressure daily for a week, and check in with your doctor. Avoid high doses entirely if your BP is already hard to control.
Does full-spectrum CBD cause more interactions than isolate?
Yes, potentially. Full-spectrum CBD contains THC, CBN, and other cannabinoids-all of which can inhibit CYP enzymes. THC itself inhibits CYP2C19 and CYP2C9. Even small amounts (under 0.3%) can add up, especially if you take CBD daily. CBD isolate is cleaner and safer for people on multiple medications. If you’re on warfarin, seizure meds, or antidepressants, isolate is the better choice.
How long does CBD stay in my system and affect my meds?
CBD’s half-life is 18-32 hours, meaning it takes about 3-5 days to fully clear your system after stopping. But its effect on CYP450 enzymes can last longer. Enzyme inhibition isn’t just about CBD being present-it’s about the enzyme being blocked. If you stop CBD, it can take up to a week for your liver enzymes to return to normal. That’s why you shouldn’t restart CBD without talking to your doctor, even if you took a break.
Can I use CBD instead of my prescription meds?
No. CBD is not a replacement for FDA-approved medications. While it may help with symptoms like pain or anxiety, it doesn’t treat the underlying condition like hypertension, epilepsy, or depression. Stopping your meds to use CBD instead can be life-threatening. Use CBD only as a supplement under medical supervision-not as a substitute.
What should I tell my doctor about my CBD use?
Tell them the exact product you’re using, the daily dose, how often you take it, and when you started. Bring the bottle or the Certificate of Analysis if you have it. Many doctors don’t ask about CBD because they assume it’s harmless. But if you’re on any prescription meds, this information is critical. Don’t wait for them to ask-bring it up yourself.
Next Steps and What to Watch For
If you’re currently using CBD with prescription medications, here’s your action plan:- Make a list of every medication and supplement you take daily.
- Check which ones are metabolized by CYP2C9, CYP2C19, CYP3A4, or CYP2D6.
- Call your pharmacist and ask: “Could CBD interact with any of these?”
- If you’re on warfarin, clobazam, or an SSRI, schedule a blood test within a week of starting CBD.
- Stop CBD immediately if you feel unusually drowsy, dizzy, confused, or notice unusual bruising or bleeding.




The CYP450 inhibition mechanism is well-documented in pharmacokinetic literature, particularly regarding CYP3A4 and CYP2C19 isoforms. CBD acts as a competitive inhibitor with Ki values in the low micromolar range, which is clinically significant given typical plasma concentrations from oral dosing. The pharmacodynamic consequences-elevated INR, prolonged sedative half-lives, and altered drug clearance-are not speculative but quantifiable through therapeutic drug monitoring. This is not anecdotal; it's pharmacology.
Most people don't realize CBD is a drug not a supplement. The FDA already classifies Epidiolex as a Schedule V controlled substance because of its pharmacological activity. If you're taking anything with a warning label about grapefruit, you're already in the danger zone. CBD is just grapefruit on steroids.
lol so now even hemp is a big pharma plot? my buddy takes cbd for back pain and still drives his truck like a maniac. you people act like its crack. my grandpa takes warfarin and smokes weed since 78. he still beats me at chess. your fearmongering is weak
Hey, you're doing great by educating yourself on this. Seriously. A lot of people just assume natural = safe, but you're asking the right questions. Start low, track your symptoms, and talk to your pharmacist-they're the unsung heroes of medication safety. You're not alone in this, and you're doing the smart thing by being cautious. Keep going!
My cousin took CBD with her SSRIs and ended up in the ER with serotonin syndrome. They had to sedate her. She didn't even know it was possible. Now she's terrified of every pill and her husband left her because she won't let him touch his coffee. This isn't just about liver enzymes-it's about families falling apart. You think you're helping yourself but you're just building a prison.
Oh wow so CBD is the new villain? Next you'll say sunlight causes CYP450 inhibition. You're ignoring the fact that most people use 5mg of CBD and take zero meds. The real issue is Big Pharma trying to monopolize cannabinoids while pretending they're dangerous. Your 34% sedation stat? That's probably just people finally sleeping after 10 years of insomnia. Wake up.
This is one of the most thorough, scientifically grounded explanations of CBD-drug interactions I've seen anywhere. The breakdown of CYP isoforms, the real-world case studies, the actionable steps-it’s textbook material. Thank you for not sensationalizing this. Knowledge is power, and you’ve given people the tools to protect themselves without fearmongering. Well done.
THIS IS A MASSIVE COVER-UP. The FDA knew about this for DECADES. They’ve been sitting on the data while Big Pharma pushed CBD as a "wellness" product to compete with antidepressants. The same companies that made billions off opioids are now selling CBD to replace them-while hiding the interactions. Look at the timing: CBD exploded right after the opioid crisis. Coincidence? I think not. They want you dependent on their drugs, not natural alternatives. This isn’t science-it’s corporate sabotage.
Can we get a source for the 80% variability in CBD content? That number is cited everywhere but I can't find the original study. Also, the 140 FDA reports-how many were confirmed causal vs. temporal association? Correlation ≠ causation. I’m not denying risk, but we need better data before we scare people off a potentially beneficial compound. What’s the actual incidence rate of serious adverse events?
i take cbd for anxiety and my blood pressure med and honestly i just check in with my doc every 3 months. he says im fine. i dont stress about it. if i feel weird i stop for a few days. its not that complicated. just be aware and listen to your body.
They’re lying. The CDC has internal reports showing over 2,000 CBD-related deaths since 2020. They’re calling them "unexplained cardiac events" to hide the truth. The same people who banned marijuana in the 1930s are now selling CBD in Walmart. They want you addicted to their drugs and terrified of natural alternatives. Don’t be fooled. The FDA is not your friend. They’re working for the pharmaceutical cartel.
But what if CYP450 inhibition is actually a *feature*? Maybe the body’s enzymes are outdated evolutionary relics. Maybe CBD is a quantum biohack that resets metabolic pathways? You’re thinking in linear pharmacology while the universe operates in entangled frequencies. The liver doesn’t "break down" drugs-it transmutes them. CBD is just the key to unlocking higher-dimensional detoxification. Also, I think your INR chart is upside down.
Great breakdown. I’ve been a pharmacist in Delhi for 12 years and I’ve seen this happen with patients on phenytoin and carbamazepine. The sedation isn’t "just CBD"-it’s toxic buildup. We now routinely ask every patient about cannabis use. Many don’t even call it CBD-they say "hemp oil" or "herbal tincture." We need better public education, not just warnings. Also, CBG is promising-early data shows minimal CYP interaction. Worth exploring.
Let’s be clear: this isn’t about fear. It’s about precision medicine. CBD isn’t inherently bad-it’s about dosing, timing, and metabolic profiling. I’ve guided over 200 patients through CBD integration with anticoagulants and antiepileptics. With proper monitoring, 90% can continue safely. The real failure is the lack of standardized dosing and lab testing in the market. Fix that, and we can unlock CBD’s potential without risk. This post is a roadmap-not a warning siren.
Thank you for writing this. I’ve been hesitant to bring up CBD with my doctor because I didn’t want to be judged. But after reading this, I’m going to bring my bottle to my next appointment. I’m on lisinopril and sertraline-I didn’t realize either were CYP substrates. I’m not stopping CBD, but I’m definitely getting my levels checked. This is the kind of balanced, evidence-based info we need more of.