Imagine waking up one day and no longer needing to take pills for your type 2 diabetes. Not because you got lucky, but because you changed your life-and your blood sugar stayed under control without them. This isn’t science fiction. It’s remission. And it’s happening more often than doctors used to think possible.
What Does Diabetes Remission Actually Mean?
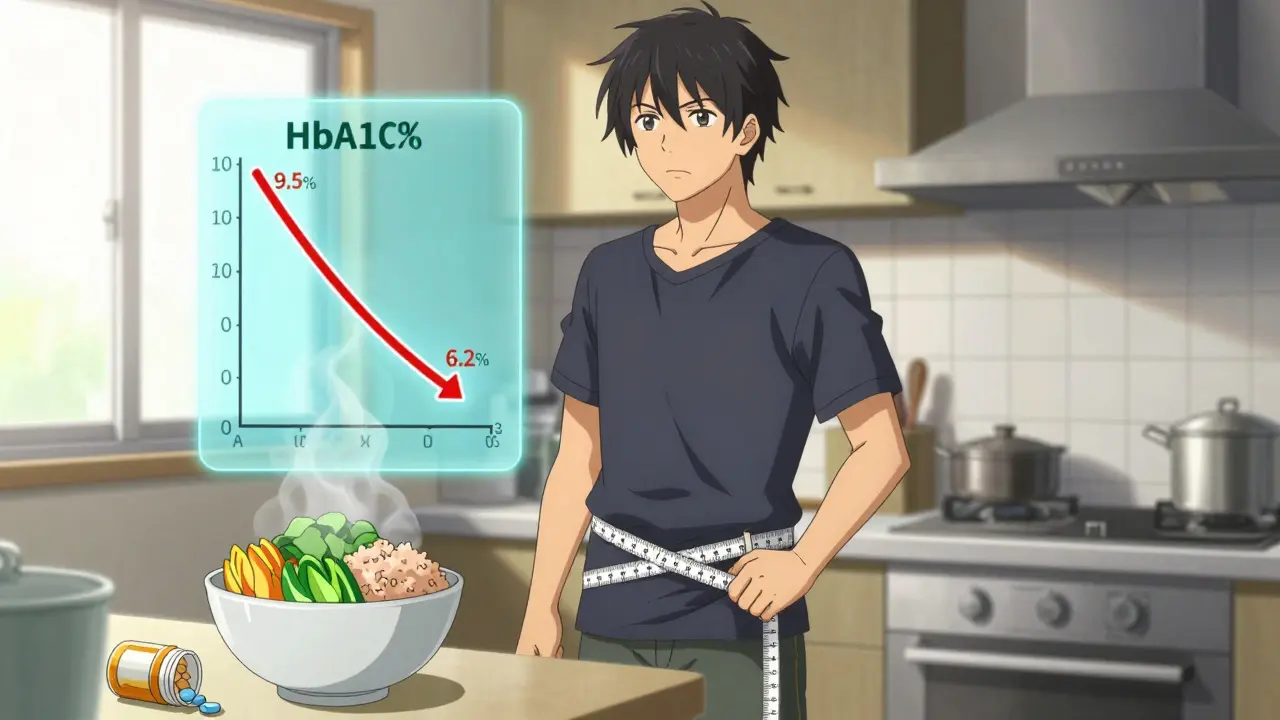
Remission in type 2 diabetes isn’t a cure. It’s not magic. It’s a measurable, documented drop in blood sugar that lasts-without meds. According to the 2021 international consensus from the American Diabetes Association, the Endocrine Society, and Diabetes UK, remission means your HbA1c stays below 6.5% (48 mmol/mol) for at least three months, and you’re not taking any diabetes medications. Not metformin. Not insulin. Not GLP-1 agonists. Nothing.This definition wasn’t pulled out of thin air. Before 2021, every study used its own rules. Some counted remission if blood sugar was normal even with pills. Others required no meds but used different timeframes. The confusion made it hard for doctors to talk to patients or compare results. Now, there’s a clear standard. And it’s practical: if you’re off meds and your HbA1c is low, you’re in remission.
But here’s the catch: if you’re still taking drugs to keep your numbers down, you don’t qualify. That’s intentional. Remission isn’t about better control with medicine. It’s about your body regaining control on its own.
How Weight Loss Makes It Happen
The biggest driver of remission? Losing weight. Not a little. Not “try to eat less.” Real, sustained weight loss-usually 10 kilograms (22 pounds) or more.The DiRECT trial, a landmark study in the UK, showed that 46% of participants who lost at least 10kg went into remission after one year. That’s nearly half. Even more striking? At two years, 36% were still in remission. That’s not a fluke. That’s proof that fat loss, especially around the liver and pancreas, can restore insulin function.
How does it work? When you carry too much fat inside your organs, it interferes with how insulin works. Your pancreas struggles to make enough, and your body stops responding to it. Lose that fat, and the pancreas can start working again. Studies using MRI scans show that people in remission have less fat in their liver and pancreas than those still on meds-even if their weight is similar.
It’s not just about the scale. It’s about where the weight comes off. Belly fat is the main culprit. That’s why waist circumference matters as much as total weight. Men with waistlines over 40 inches and women over 35 inches are at much higher risk for insulin resistance. Dropping even a few inches can make a big difference.
Who Has the Best Chance?
Not everyone gets remission. But some people have a much better shot.If you’ve had type 2 diabetes for less than five years, your odds jump significantly. Why? Because your pancreas hasn’t been worn down yet. Beta cells-the insulin-producing cells-are still alive and can recover if the stress of excess fat is removed.
People who don’t need insulin are also more likely to succeed. Insulin use often means the pancreas has lost a lot of its function. It’s harder to bounce back. Those still on oral meds like metformin have better outcomes than those on insulin.
And your starting HbA1c matters. If you’re at 7.5% instead of 9.5%, you’re already closer to the target. Less ground to cover. Less weight to lose. Less time to wait.
Age? Doesn’t matter as much as you’d think. People in their 60s and 70s have achieved remission too. It’s not about being young. It’s about being consistent.
What Happens When You Stop Medication?
Going off meds sounds scary. And it should be done carefully.You don’t just stop taking your pills one day and hope for the best. Your doctor needs to monitor your blood sugar closely as you reduce or stop medication. This usually happens after you’ve started losing weight and your numbers begin to drop. Some people taper off metformin slowly. Others stop insulin under strict supervision.
Why? Because if you drop your meds too fast, your blood sugar can spike. That’s dangerous. But if you wait too long, you might miss the window where your body can recover. The timing is everything.
Once you’re off meds and your HbA1c is under 6.5% for three months, your doctor will confirm remission. But you’re not done. You still need checkups. At least once a year. Because remission can fade.
Remission Isn’t Permanent-But It’s Worth It
About half the people who reach remission eventually see their blood sugar rise again. That’s not failure. It’s biology.Your body didn’t forget how to work. It just got tired. If you gain weight back, the fat returns to your organs. The insulin resistance creeps back in. But even if you relapse, you’re not starting from scratch. You’ve already proven your body can recover. You’ve bought yourself time. And time reduces complications.
Studies show that spending even a year or two in remission lowers your risk of nerve damage, kidney disease, and heart problems. That’s huge. One extra year without high blood sugar means fewer damaged blood vessels. Fewer hospital visits. Fewer meds down the road.
Dr. Roy Taylor from Newcastle University puts it simply: “Remission doesn’t mean you’re cured. But it means you’ve taken back control.”
How to Actually Do It
So how do you get there?- Focus on weight loss, not just dieting. Aim for 10kg or more. That’s the magic number from the research.
- Use proven methods. Total diet replacement programs (like meal replacements for 12 weeks) have worked in clinical trials. So have low-carb diets and Mediterranean eating patterns. Pick what you can stick with.
- Move daily. Walking 10,000 steps a day helps. Strength training twice a week helps more. Muscle burns fat-even when you’re sitting.
- Work with a team. A dietitian, a diabetes educator, or a lifestyle coach can make the difference between trying and succeeding. Don’t go it alone.
- Track your progress. Measure your HbA1c before you start. Check it every 3 months. Watch your waist size. Keep a food and activity log.
Some people try fasting. Others use GLP-1 medications like semaglutide to jump-start weight loss. That’s okay-but remember: if you’re still on meds when your HbA1c drops, you’re not in remission. The goal is to get off them.

What Doctors Are Saying Now
Gone are the days when doctors said, “You’ll be on this for life.” The American College of Lifestyle Medicine now has official guidelines for using diet and exercise to treat and reverse type 2 diabetes. The NHS in Scotland has patient resources titled “Remission: Stop Diabetes in Its Tracks.”Doctors are no longer just treating blood sugar numbers. They’re treating the root cause: excess fat. And they’re celebrating when patients get off meds.
Dr. Michael Nauck, a leading endocrinologist, warns: “Don’t stop medications just because you want remission. If your meds are keeping you safe, keep taking them. But if you’re losing weight and your numbers are improving, talk to your doctor about a plan to reduce them.”
That’s the new mindset: remission isn’t an all-or-nothing goal. It’s a path. And it’s open to more people than ever before.
What You Should Know Before You Start
Remission is powerful. But it’s not risk-free.- It’s not a cure. Your body still has the same underlying tendency toward insulin resistance. You just turned it down.
- Complications don’t vanish overnight. If you had high blood sugar for years, you might still have nerve or eye damage. Remission slows further damage-but doesn’t reverse what’s already there.
- Long-term data is still limited. We don’t know yet if remission reduces death rates. But we do know it improves quality of life.
- Relapse is common. Don’t see it as failure. See it as a sign to recommit.
The biggest mistake people make? Thinking remission means they can go back to old habits. You can’t. You’ve proven you can change. Now you have to keep doing it.
Final Thought: This Is Your Body’s Way of Saying ‘Thank You’
Type 2 diabetes isn’t a punishment. It’s a signal. Your body is telling you it’s overwhelmed. Lose the weight. Move more. Eat real food. And for many people, it responds-not with a miracle, but with a second chance.Remission isn’t about perfection. It’s about persistence. One meal at a time. One walk at a time. One pound lost at a time.
And when your HbA1c drops below 6.5% without a single pill? That’s not just a number. That’s freedom.
Can type 2 diabetes be reversed without surgery?
Yes. Surgery (like gastric bypass) can lead to remission in about 37% of cases, but non-surgical weight loss through diet and lifestyle changes has also proven effective. The DiRECT trial showed 46% remission after one year with intensive weight loss-no surgery needed. The key is losing at least 10kg and keeping it off.
How long do you need to be off medication to qualify for remission?
You must be off all glucose-lowering medications for at least three months, with HbA1c consistently below 6.5% during that time. This is the international standard set by the ADA, EASD, and Diabetes UK in 2021. Testing before and after stopping meds is required to confirm remission.
Is remission possible if I’m on insulin?
It’s much harder, but not impossible. Insulin use usually means your pancreas has lost most of its insulin-producing ability. Still, some people have achieved remission after significant weight loss, even after insulin. However, most successful cases come from people who haven’t needed insulin. If you’re on insulin, focus on weight loss first, then work with your doctor to safely reduce meds.
Will I need to check my blood sugar after remission?
Yes. Even in remission, you should have your HbA1c checked at least once a year. Blood sugar can creep back up if weight is regained. Regular monitoring helps catch a relapse early. You should also keep seeing your doctor for other diabetes-related checks, like eye and kidney exams.
Can I eat carbs again if I’m in remission?
You can, but you’ll need to be careful. Remission doesn’t mean your body suddenly tolerates large amounts of sugar and refined carbs. Most people who stay in remission follow a balanced, whole-food diet-lower in processed carbs and added sugars. Portion control and timing matter. Eating a large pizza or drinking soda regularly will likely bring your blood sugar back up.
Does losing 5kg help with remission?
Losing 5kg may improve your blood sugar and reduce medication needs, but it’s usually not enough for full remission. The research shows that 10kg or more is the threshold for the best chance of remission. That said, every pound lost helps. Even smaller losses reduce insulin resistance and lower your risk of complications.
Is remission possible for older adults?
Yes. Age isn’t a barrier. People in their 60s and 70s have achieved remission through weight loss and lifestyle changes. What matters more than age is how long you’ve had diabetes, your starting weight, and your ability to stick with changes. Many older adults benefit even more because they’re motivated to avoid complications and stay independent.






So basically if you lose weight your pancreas magically starts working again? Sounds like a miracle cure but everyone knows diabetes is lifelong no matter what you do. I’ve seen too many people think they’re cured then end up in the hospital. Don’t fall for the hype.
Of course it works. We’ve known this for decades. The British medical establishment just finally caught up. Americans still think pills fix everything. Pathetic.
This gave me chills 😭 I’ve been in remission for 14 months now-no meds, HbA1c 5.8, and I walk 10k steps every day. It’s not easy but it’s worth every sweat drop. You got this!! 💪
Let’s be clear: remission is not reversal. You are still diabetic. You’ve merely delayed the inevitable by temporarily reducing fat mass. The moment you eat a bagel, your beta cells collapse again. This is not empowerment-it’s delusion dressed up as science.
I love how this article doesn’t shame anyone. It just says: lose weight, move more, work with your team. No magic pills. No quick fixes. Just real life. And that’s enough. Seriously-this is hope without hype.
My dad’s been in remission for 3 years now. He didn’t do anything crazy-just stopped soda, started walking after dinner, and got his HbA1c checked every 6 months. He’s happier, sleeps better, and doesn’t feel like a patient anymore. It’s not perfect but it’s real.
My doctor said I’d be on metformin forever. I lost 12kg over 8 months with a low-carb Mediterranean diet and now I’m off everything. My HbA1c is 5.9. I don’t celebrate it like a trophy-I celebrate it like a second chance. And yeah, I still eat carbs. Just not the crap that makes me sick.
The DiRECT trial results are compelling, but generalizing them to all populations is problematic. The cohort was primarily white, middle-class, and highly motivated. In lower-income communities, access to dietitians, meal replacements, and time for exercise is limited. Remission is possible-but equity in access remains a critical, unaddressed barrier.