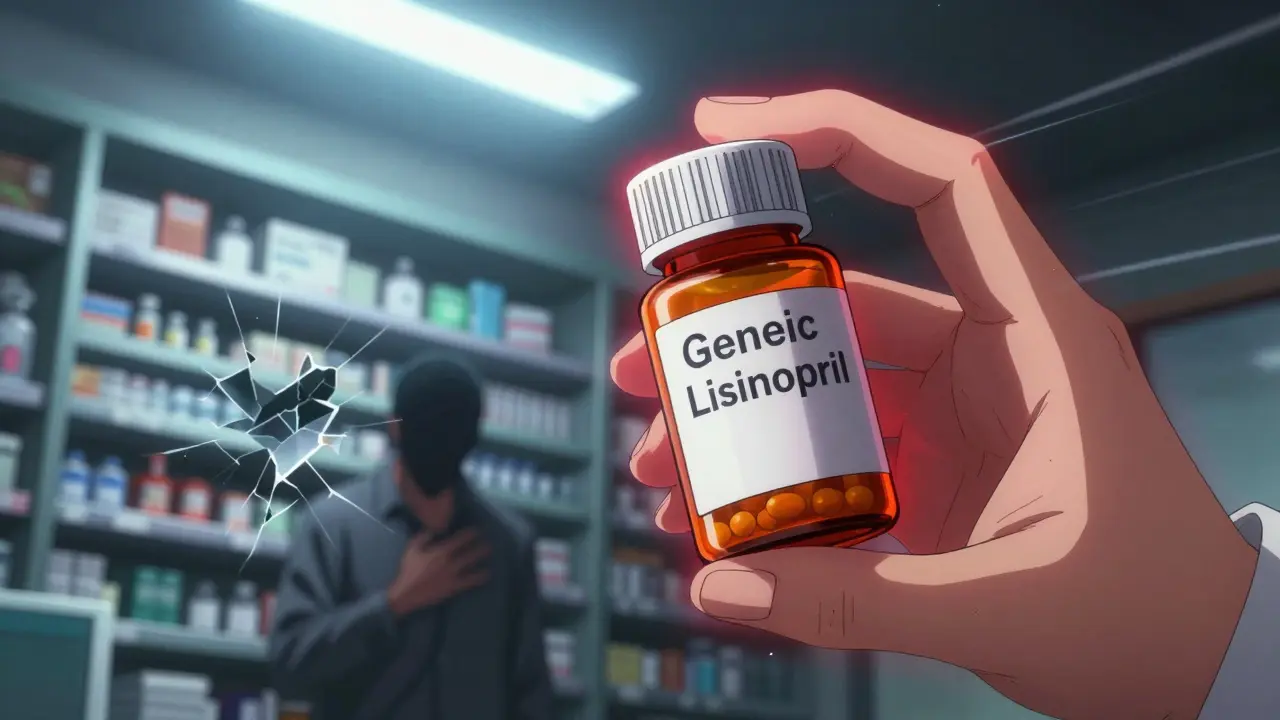
More than 9 out of 10 prescriptions in the U.S. are filled with generic drugs. They’re cheaper, widely available, and trusted. But right now, many of these essential medicines are disappearing from pharmacy shelves - not because of demand, but because of broken economics and fragile supply chains. If you or someone you know takes medication for high blood pressure, thyroid issues, antibiotics, or even cancer, you’ve likely felt the impact. This isn’t a temporary glitch. It’s a systemic collapse hidden in plain sight.
The myth of cheap and easy
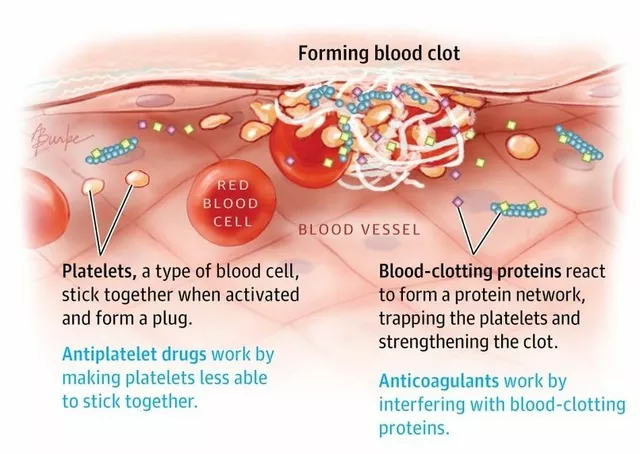
People assume generic drugs are simple to make. After all, they’re copies of brand-name pills. But making a safe, effective generic isn’t just mixing chemicals. It’s a high-stakes, precision process that requires sterile environments, exact formulations, and flawless quality control. The problem isn’t the science - it’s the money. Generic manufacturers operate on margins as thin as 5% for some drugs. That’s not profit. That’s survival. Compare that to branded drug companies, which often make 70-80% gross margins. When a new company enters the market and undercuts prices by a fraction of a cent per pill, the whole system collapses. Manufacturers can’t afford to upgrade equipment, hire enough staff, or even keep their factories running. So they shut down.Where your medicine is really made
Chances are, the active ingredient in your generic medication was made in India or China. The FDA says 72% of all drug manufacturing facilities that supply the U.S. are overseas. For critical drugs like antibiotics, 97% of the active ingredients come from outside the U.S. For antivirals, it’s 92%. Even common pain relievers like acetaminophen rely on raw materials mostly sourced from China. This global web of suppliers sounds efficient - until something breaks. During the pandemic, India halted exports of 26 essential medicines. Factories in China shut down. Suddenly, hospitals ran out of antibiotics, heart meds, and even epinephrine. There were no backups. No domestic production. No stockpiles. Just silence. The supply chain isn’t linear. One company makes the active ingredient. Another mixes it with fillers. A third coats the pill. A fourth packages it. Each step happens in a different country. One delay, one inspection failure, one quality issue - and the whole chain stops.Quality control is failing
The FDA inspects foreign facilities less often than domestic ones. Even when they do, many manufacturers don’t meet U.S. standards. In 2022, the FDA pulled Intas Pharmaceuticals’ cancer drug cisplatin from the U.S. market after finding "enormous and systematic quality problems." The company had been shipping contaminated or improperly labeled batches for years. A 2023 study found generic drugs made in India had 54% more serious adverse events - including hospitalizations and deaths - compared to identical drugs made in the U.S. That doesn’t mean all Indian-made drugs are dangerous. But it does mean the system isn’t catching problems before they reach patients. Documentation is another issue. U.S. manufacturers keep 95%+ accurate batch records. Some foreign facilities hover around 78%. One missing record, one unreported deviation, one uncleaned machine - and an entire batch gets recalled. The cost? $1.7 million per facility to fix. Many can’t afford it.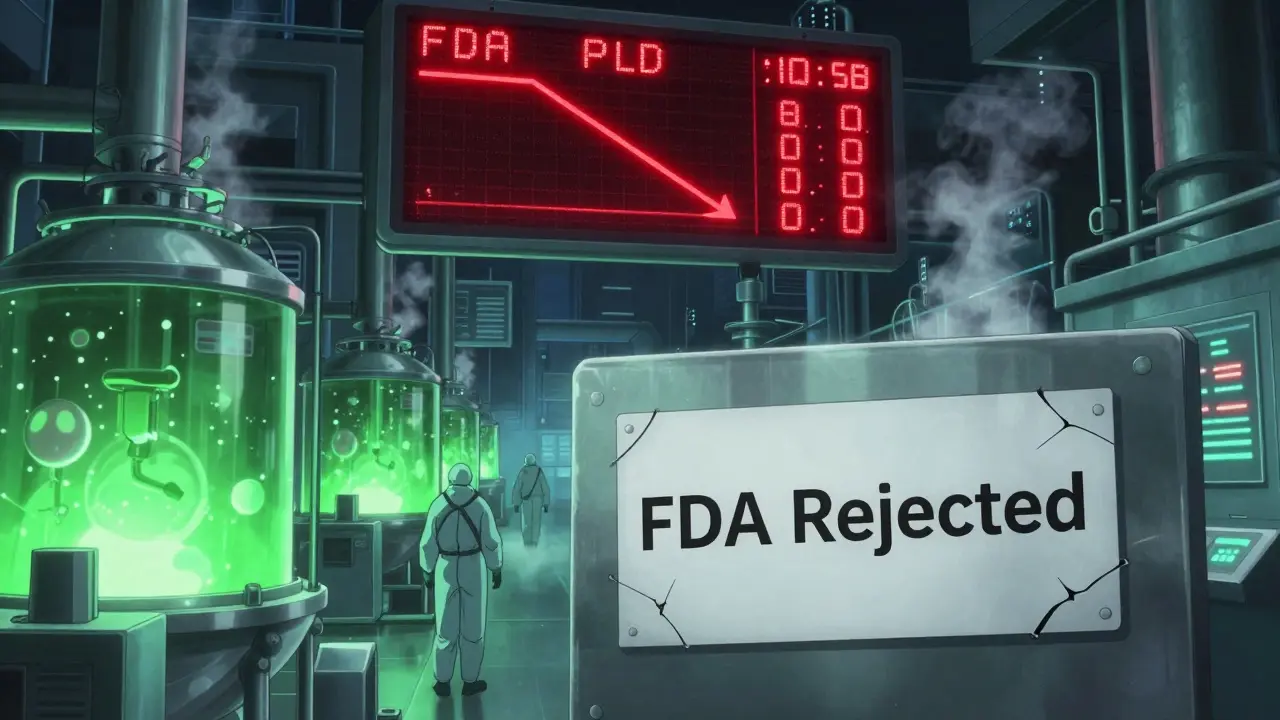
Why no one builds factories here
Building a single FDA-approved manufacturing plant in the U.S. costs between $250 million and $500 million. It takes 3 to 5 years. In India or China? $50 million to $100 million. Same output. Half the time. Same regulations? Not really. Foreign countries often have looser oversight, faster approvals, and lower labor costs. Even if a U.S. company wanted to invest, the market punishes them for it. Group purchasing organizations (GPOs) and pharmacy benefit managers (PBMs) award contracts based on price alone - sometimes choosing a drug that’s 0.001 cents cheaper per tablet. There’s no reward for quality. No bonus for reliability. No penalty for supply failures. So why spend $500 million to build a plant here when you can buy a cheaper, riskier product from overseas and still win the contract?The race to the bottom
This isn’t just about cost. It’s about incentives. Every time a new generic manufacturer enters the market, they undercut the existing players. Prices drop. Margins shrink. The original manufacturer can’t compete. They stop making the drug. Then the new player gets squeezed too. Eventually, no one makes it. That’s what happened to Akorn Pharmaceuticals. They went bankrupt in 2023 and stopped producing 200+ drugs overnight. No one had backup supply. Patients were left without treatments for epilepsy, cancer, and heart conditions. The system didn’t have a Plan B - because it never needed one. The market has shrunk dramatically. In 2010, 35% of active pharmaceutical ingredients were made in the U.S. By 2023, that number dropped to 14%. Over 37% of U.S.-based generic manufacturers have closed or idled their facilities in the last decade. Only five companies now control nearly half the market. That’s not competition. That’s consolidation - and it’s making the system even more fragile.







They shut down the last US penicillin plant in 2012. We used to make 90% of our own antibiotics. Now we import 97%. That’s not globalization. That’s surrender.
in india we make these pills with pride but no one pays us enough to fix the machines
we want to do better but the price keeps dropping
its not our fault the system is broken
Let’s be real. If we let China and India run our medicine supply, we’re one pandemic away from mass death. This isn’t capitalism. This is national suicide. Build the plants here. Now. Or we’re all just waiting for the next crisis.
Did you know the FDA gets paid by the pharma companies they inspect? That’s why they keep greenlighting dirty factories. This isn’t a shortage. It’s a cover-up. The same people who sold you the pills are hiding the truth.
you think this is bad? wait till the next bioterror attack hits and we cant find a single batch of epinephrine that isnt contaminated
they’ve been skipping sterility tests since 2018 and no one cares
the FDA reports are falsified
ask your pharmacist if they know where your pills came from
they probably dont
Let me just say this with the precision of a toxic analyst: the entire generic drug ecosystem is a Ponzi scheme built on regulatory arbitrage. We’ve outsourced not just manufacturing but ethical responsibility. The FDA’s inspection backlog? It’s not a bureaucratic glitch-it’s a deliberate policy of neglect to preserve low consumer prices. And guess who pays the price? The elderly. The immunocompromised. The uninsured. We’ve turned medicine into a commodity, and now we’re reaping the corpses. The 5% margin isn’t a business model-it’s a death sentence wrapped in a pill.
so we pay $0.02 for a pill made in a factory with no running water
and then act shocked when it doesn’t work
the system is literally designed to fail
and we wonder why people are dying
lol
you think america is the victim here? we make your pills and you call us dirty? you dont pay us enough to fix the air filters
we are not villains we are survivors
you want clean medicine? pay for it
or shut up
all this drama about pills
just take the brand name if you can afford it
or dont complain when you run out
we’ve been making these for decades
the problem is you want cheap and perfect
thats not how the world works
The moral architecture of pharmaceutical policy has collapsed under the weight of utilitarianism. When we reduce life-sustaining medicine to a line item on a balance sheet, we do not achieve efficiency-we achieve moral bankruptcy. The absence of domestic production is not an economic choice; it is a cultural failure of foresight, solidarity, and civic responsibility. To restore integrity to this system, we must decouple access from price, incentivize quality over cost, and treat pharmaceutical manufacturing as critical infrastructure-not a market niche. The alternative is not a shortage of drugs. It is a shortage of conscience.
the fact that we have 278 drug shortages and no one in congress is making this a top priority… 😔