Heartburn hits hard - a burning sensation in your chest, a sour taste in your mouth, maybe even trouble sleeping. If you’ve ever reached for a bottle of Tums, Pepcid, or Prilosec without a prescription, you’re not alone. Nearly 60 million Americans deal with heartburn at least once a month. But not all OTC heartburn meds work the same way. Choosing the wrong one can mean wasted money, wasted time, or worse - side effects you didn’t expect.
How Antacids Work (and When They’re Actually Useful)
Antacids are the OG heartburn fix. They’ve been around since the 1800s. Think of them like a chemical sponge for stomach acid. They don’t stop acid production - they neutralize it right where it is. That’s why they work so fast.
If you just ate spicy food and feel the burn starting, an antacid like Tums (calcium carbonate) can knock out the pain in under a minute. Milk of Magnesia (magnesium hydroxide) and Alternagel (aluminum hydroxide) work the same way. You chew or swallow, and within 30 to 120 seconds, relief kicks in.
But here’s the catch: it doesn’t last. Most antacids only work for 30 to 60 minutes. That’s why people who take them often end up with a handful of pills by dinner. One study found that 63% of users complain about needing to redose constantly. That’s not a flaw - it’s how they’re designed.
Antacids are perfect for occasional heartburn - less than once a week. They’re cheap, widely available, and safe for short-term use. But if you’re using them daily, you’re treating the symptom, not the cause. And some types can backfire. Calcium carbonate, for example, can trigger rebound acid hypersecretion in about 30% of users. That means your stomach makes even more acid after the antacid wears off, making heartburn worse later.
H2 Blockers: Slowing Down the Acid Factory
H2 blockers - like Pepcid AC (famotidine), Tagamet HB (cimetidine), and Axid AR (nizatidine) - work differently. Instead of mopping up acid, they tell your stomach to make less of it. They block histamine, a chemical that signals your stomach to pump out acid.
They take longer to work - usually 60 to 180 minutes - but their effects last much longer: 8 to 12 hours. That’s why they’re popular for predictable heartburn. If you know you’ll eat pizza on Friday night, take a Pepcid 60 to 90 minutes before. You’re less likely to feel the burn later.
Studies show H2 blockers reduce acid production by about 60-70%. That’s not as strong as PPIs, but it’s enough for people who get heartburn 1-2 times a week. The American Gastroenterological Association recommends them as a first choice for this group.
But there’s a downside. After 2-3 weeks of daily use, your body can start to build tolerance. The same dose stops working as well. That’s why many users on Reddit and Drugs.com report that H2 blockers “stop working after a couple weeks.”
They also interact with other meds. Cimetidine can interfere with blood thinners like warfarin and seizure meds like phenytoin. Always check with a pharmacist if you’re on other prescriptions.
PPIs: The Heavy Hitters - Powerful, But Not for Everyone
Proton pump inhibitors - Prilosec OTC (omeprazole), Nexium 24HR (esomeprazole), and Prevacid 24HR (lansoprazole) - are the strongest OTC heartburn meds you can buy without a prescription. They shut down the acid pumps in your stomach cells completely. That’s why they suppress acid by 90-98%.
But here’s the twist: they don’t work fast. You won’t feel relief after one pill. It takes 24 to 72 hours to reach full effect. That’s why so many people give up on them too soon. One user on Amazon wrote, “I took it for two days and nothing happened. I threw it out.” That’s a common mistake.
PPIs are meant for frequent heartburn - two or more days a week. If you’re having heartburn every day, or waking up at night with it, a PPI is the only OTC option that can truly help. A 2022 JAMA study found PPIs reduced symptoms by 90% over 14 days. H2 blockers? Only 65%.
But they come with serious warnings. The FDA requires a boxed warning on all OTC PPIs about increased risk of Clostridium difficile infection (a severe gut infection) and hip fractures with long-term use. Studies also link daily PPI use to lower magnesium and vitamin B12 levels, kidney disease, and even pneumonia.
And timing matters. You must take PPIs before food - ideally 30 to 60 minutes before breakfast. If you take them after eating, or with orange juice (which breaks down the coating), they won’t work. One user on r/gerd said, “I used to take mine at night. Didn’t help. Then I started taking it before breakfast - game changer.”
And you’re not supposed to take them longer than 14 days in a row. The FDA made that rule for a reason. If your heartburn comes back after 14 days, you need to see a doctor - not just take another pack.
Which One Should You Choose?
It’s not about what’s “best.” It’s about what fits your pattern.
- Occasional heartburn (less than once a week)? Start with an antacid. Chew a Tums. You’ll feel better fast. Just don’t make it a habit.
- Predictable heartburn (1-2 times a week)? Try an H2 blocker. Take Pepcid 60 minutes before your trigger meal. It’s reliable, affordable, and works for most people.
- Frequent heartburn (two or more days a week)? A PPI is your best bet. But only use it for 14 days straight. If symptoms return, see a doctor. Don’t just buy another bottle.
Many people combine them. About 68% of frequent heartburn sufferers use an antacid for instant relief and a PPI for long-term control. That’s smart - if you do it right. Don’t take antacids and PPIs at the same time. Wait at least two hours. Antacids can interfere with how PPIs are absorbed.
What No One Tells You About OTC Heartburn Meds
Here’s the truth: OTC heartburn meds are not a cure. They’re a bandage. If you’re relying on them for months or years, something deeper is going on. GERD isn’t just “too much acid.” It’s often a weak lower esophageal sphincter, hiatal hernia, or even a food sensitivity.
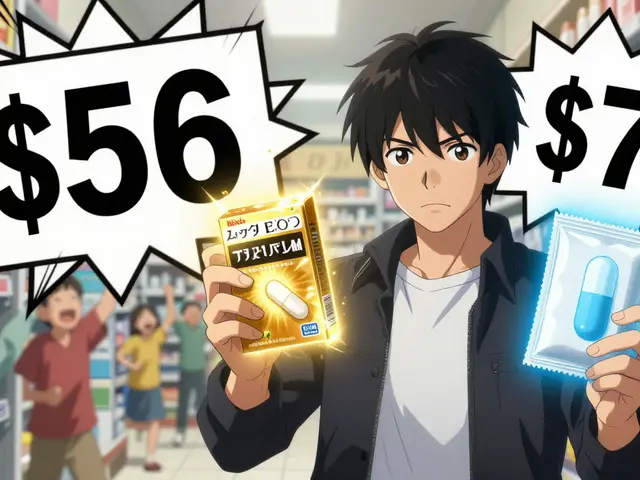
Also, cost isn’t always a clue to quality. Generic PPIs now make up 68% of sales. Curist’s generic omeprazole costs $4.99 - less than a coffee. The brand-name version? $24.99. Same active ingredient. Same results.
And don’t ignore lifestyle. Losing 10 pounds can cut heartburn in half. Avoiding late-night meals, caffeine, and alcohol helps more than any pill. But if you’re already doing all that and still burning - it’s time to talk to a doctor. No OTC pill should be your permanent solution.
What to Do Next
Start by tracking your symptoms. How often? When? What triggers it? Write it down for a week. Then match it to the right OTC option.
- Once a week or less? Antacid.
- 1-2 times a week, same time each day? H2 blocker.
- Two or more days a week? PPI - but only for 14 days. Then stop and reassess.
If you’ve tried all three and still have symptoms - or if you have trouble swallowing, unexplained weight loss, or vomiting blood - stop self-treating. See a doctor. You could have GERD, a hiatal hernia, or something more serious.
And if you’re already on a PPI for more than 14 days? Talk to your pharmacist. Ask if you’re using it correctly. Ask if you need a different approach. You don’t need a prescription to get advice - just a conversation.
Can I take antacids and PPIs together?
Yes, but not at the same time. Antacids can interfere with how PPIs are absorbed. Wait at least two hours between taking an antacid and a PPI. Use the antacid for immediate relief and the PPI for long-term control.
Why doesn’t my PPI work right away?
PPIs don’t neutralize acid - they shut down the acid-producing pumps in your stomach. Those pumps need time to be fully inhibited. It takes 24 to 72 hours to reach maximum effect. Don’t give up after one or two doses. Take it daily for at least three days before judging.
Are generic PPIs as good as brand names?
Yes. Generic omeprazole, esomeprazole, and lansoprazole are bioequivalent to their brand-name versions. The FDA requires them to deliver the same amount of active ingredient into your bloodstream. Curist and other generics cost up to 80% less and work just as well.
Can I take H2 blockers every day?
You can, but not for long. After 2-3 weeks, your body often becomes less responsive. H2 blockers are best for occasional or predictable use - not daily maintenance. If you need daily relief for more than a few weeks, talk to a doctor about PPIs or other options.
Is heartburn ever dangerous?
Occasional heartburn is common. But if you have trouble swallowing, unexplained weight loss, vomiting blood, or black stools, it could be a sign of esophagitis, Barrett’s esophagus, or even cancer. Don’t ignore these symptoms. See a doctor immediately.
What’s the safest long-term option?
There’s no truly safe long-term OTC heartburn medication. Antacids have the fewest risks but don’t last. H2 blockers lose effectiveness. PPIs carry known long-term risks. The safest long-term strategy is lifestyle changes - weight loss, avoiding trigger foods, not eating before bed - and using meds only as needed, under a doctor’s guidance.
Final Thought: Don’t Just Pop Pills - Understand Why
Heartburn isn’t just about what you eat. It’s about how your body handles it. OTC meds give you control - but only if you use them right. Know your symptoms. Know your options. Know your limits. And when in doubt, talk to someone who knows more than the bottle does.









Been on PPIs for 3 years. Lost 40 pounds, stopped eating after 7pm, cut out coffee and spicy food. Still need the pill. My doctor says it's structural, not lifestyle. I don't care why it happens, I just need to not feel like I'm swallowing fire every night.
It's wild how we treat symptoms like problems instead of signals. Heartburn isn't your stomach being too acidic-it's your body screaming that something's out of balance. Maybe your diet, maybe stress, maybe your gut flora is dead. Pills just mute the alarm. But the house is still on fire.
I used to pop Tums like candy. Then I started journaling what I ate and when the burn hit. Turned out it wasn't the pizza-it was the late-night protein shake. Changed that, and my heartburn vanished. No meds needed.
We're so quick to fix the symptom that we forget to ask why it's there. The body doesn't lie. It just speaks in discomfort when we won't listen.
Antacids? Fine for a one-off. H2 blockers? Good for planning. PPIs? Only if you're ready to face the root. Otherwise, you're just delaying the reckoning.
And yeah, generics work just as well. No need to pay for marketing. The active ingredient doesn't care if it's in a $24 bottle or a $5 one.
But if you're still burning after 14 days? That's not a refill issue. That's a ‘go see someone who actually knows what they’re doing’ issue.
Stop treating your body like a machine that needs a reset button. It's a living system. Treat it like one.
PPIs take days to work? I gave up after one day.
So let me get this straight-you're telling me the FDA is right about PPIs causing fractures and infections, but we're supposed to trust a bunch of Reddit users who say ‘I took it before breakfast and it worked’? That’s not science, that’s anecdotal superstition.
And why is everyone acting like antacids are harmless? Calcium carbonate causes rebound acid. That’s not a feature, it’s a trap. You’re training your stomach to overproduce. It’s like giving a junkie a hit so they don’t go cold turkey-except you’re the junkie.
And H2 blockers ‘stop working’? Of course they do. Your body adapts. That’s biology, not failure. You’re not special because you need a stronger drug. You’re just human.
The real problem? We treat heartburn like a nuisance instead of a warning sign. And then we blame the meds when they don’t fix our terrible habits.
EVERYTHING IN THIS POST IS CORRECT. EVERY. SINGLE. WORD. AND YET, PEOPLE STILL BUY BRAND-NAMED PPIs FOR $25 WHEN THE GENERIC IS $5. AND THEY STILL TAKE ANTACIDS DAILY. AND THEY STILL EAT MIDNIGHT TACOS. THIS IS WHY AMERICA IS BROKEN. WE WANT QUICK FIXES AND WE REFUSE TO ACCEPT RESPONSIBILITY. THE FDA WARNINGS ARE THERE FOR A REASON. BUT NOBODY READS THEM. THEY JUST CLICK ‘BUY NOW’ ON AMAZON. WE’RE A NATION OF SELF-DESTRUCTIVE IDIOTS WHO THINK A PILLS CAN FIX A LIFESTYLE.
AND YES, I’M TALKING TO YOU, THE PERSON WHO JUST SCROLLED PAST THIS TO BUY MORE TUMS.
you know what they dont tell you? the ppi's are made by big pharma to keep you hooked. they put something in it that makes your body crave acid. its all a scam. the real cause is 5g towers and chemtrails messing with your stomach lining. i stopped taking everything and started drinking apple cider vinegar with honey and my heartburn vanished. also i wear a copper bracelet now. it works.
I get what everyone’s saying. But I think we’re all missing the point a little. Heartburn isn’t about being right or wrong about meds. It’s about being kind to yourself.
I used to feel guilty for needing PPIs. Like I failed because I couldn’t just ‘eat better.’ But my job is insane, I work 12-hour shifts, I’m a single dad. I don’t have time to meal prep or meditate or go on a cleanse.
So I take a generic omeprazole before breakfast. I still eat fast food sometimes. I still have coffee. But I don’t eat right before bed. And I try to walk after dinner. That’s enough.
It’s not perfect. But it’s sustainable. And that’s better than pretending you can live like a health influencer when your life looks nothing like theirs.
Use what works. Don’t shame yourself. And if it stops working? Talk to someone. Not Reddit. A real person.
Let me be perfectly clear: if you are relying on OTC heartburn medications beyond a few weeks, you are not just ignoring your health-you are actively participating in your own deterioration. This isn’t a matter of ‘personal choice’ or ‘lifestyle flexibility.’ It’s a moral failing. You are choosing convenience over consequence, ignorance over responsibility, and self-indulgence over self-preservation.
The body is not a machine to be hacked with chemical bandaids. It is a sacred vessel, and you are desecrating it with every antacid you chew, every H2 blocker you pop, every PPI you swallow without consulting a professional. You think you’re saving time? You’re wasting years. You think you’re saving money? You’re paying with your kidneys, your bones, your microbiome.
And don’t even get me started on the people who think generics are ‘just as good.’ They are identical in chemical composition, yes-but the manufacturers are not. The fillers, the binders, the manufacturing standards vary. You are gambling with your physiology on a $4.99 gamble. That is not wisdom. That is recklessness dressed up as frugality.
And yet, you still eat the nachos. You still drink the wine at midnight. You still lie down with a full stomach and then wonder why you’re burning. The answer is not in a bottle. It’s in your choices. And you are too weak to face them.
Stop blaming the pills. Start blaming yourself.
The clinical data on PPIs is robust, but the public discourse is dangerously oversimplified. The 90-98% acid suppression is pharmacologically accurate, but the temporal dynamics of proton pump inhibition are frequently misunderstood. The delayed onset of action is due to the requirement for active drug accumulation within the parietal cell canaliculi, which necessitates multiple dosing cycles to achieve steady-state inhibition.
Furthermore, the FDA’s boxed warnings regarding C. diff and hip fractures are epidemiologically significant, particularly in populations with prolonged exposure (>1 year) and concomitant corticosteroid use. However, the risk-benefit ratio remains favorable for patients with confirmed GERD or Barrett’s esophagus.
What’s often omitted in lay commentary is the importance of dosing timing relative to gastric pH cycling. PPIs are prodrugs activated in an acidic environment; ingestion prior to the first meal of the day aligns with peak pump activity, maximizing bioavailability. Concurrent antacid use can indeed reduce efficacy by elevating gastric pH prematurely.
Generic equivalence is bioequivalent per FDA 21 CFR 320, but real-world adherence and formulation variability may impact therapeutic outcomes. Clinical judgment remains paramount.
Ultimately, the most effective intervention remains lifestyle modification. Weight loss, elevation of the head of the bed, and avoidance of nocturnal ingestion are underutilized, non-pharmacological pillars of management. Medication should be adjunctive-not definitive.
As a medical professional with over 18 years of clinical experience, I must emphasize that this article, while superficially accurate, dangerously underrepresents the long-term consequences of OTC PPI overuse. The data on hypomagnesemia, vitamin B12 deficiency, and increased risk of pneumonia are not theoretical-they are documented in peer-reviewed journals including The Lancet and JAMA Internal Medicine.
Patients who self-prescribe PPIs for more than 14 days are not ‘managing’ their condition-they are masking symptoms of potential esophageal pathology. The absence of alarm symptoms does not equate to absence of disease. Silent GERD can progress to Barrett’s esophagus without warning.
Moreover, the notion that ‘antacids are fine for occasional use’ is misleading. Chronic calcium carbonate use leads to milk-alkali syndrome, which presents as acute kidney injury and metabolic alkalosis. This is not hypothetical-it is a documented emergency department diagnosis.
Furthermore, the recommendation to ‘see a doctor’ is insufficient. Patients need structured follow-up protocols, not vague advice. A simple referral to a gastroenterologist after 14 days of continuous PPI use should be standard. Instead, we have a $10 billion OTC market built on ignorance.
Stop treating this like a consumer product. This is a clinical condition. And your body is not a vending machine.