What Is Anaphylaxis?
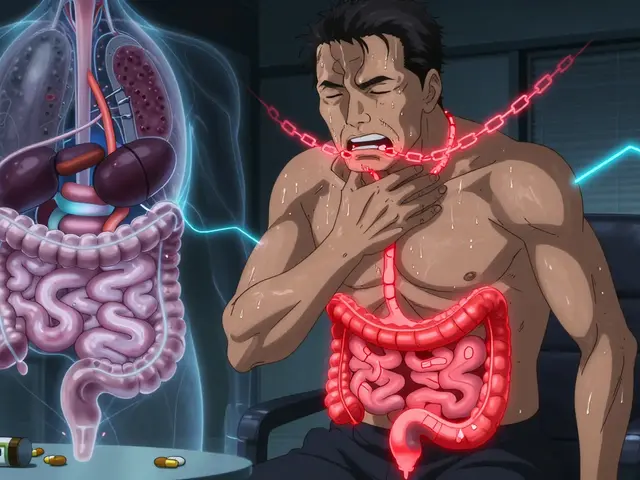
Anaphylaxis is a sudden, life-threatening allergic reaction that can shut down breathing, drop blood pressure, and cause death within minutes if not treated. It doesn’t start with a sneeze or a rash-it hits fast. One moment you’re fine; the next, your throat is closing, your skin is breaking out in hives, and you’re struggling to breathe. This isn’t just a bad allergy. It’s a medical emergency.
Anaphylaxis happens when your immune system overreacts to something harmless-like peanuts, bee stings, or penicillin-and floods your body with chemicals that cause widespread inflammation. The reaction can begin in seconds or take up to two hours, but symptoms usually appear within 5 to 30 minutes after exposure. About 1.6% of people in the U.S. have had anaphylaxis at least once, and the number is rising, especially among children.
How to Spot Anaphylaxis Early
Knowing the signs can save a life. Anaphylaxis doesn’t always look the same, but it almost always involves problems with breathing, circulation, or both. The most common symptoms include:
- Itchy skin, hives, or swelling of the lips, tongue, or throat
- Wheezing, coughing, or trouble breathing
- Dizziness, fainting, or a sudden drop in blood pressure
- Nausea, vomiting, or stomach cramps
- Rapid or weak pulse
Eight out of ten people will have skin symptoms like hives or swelling. But here’s the catch: you don’t need a rash to have anaphylaxis. Some people-especially adults-go straight to breathing or heart problems without any visible skin changes. That’s why waiting for a rash to appear before acting is deadly.
If someone has been exposed to a known allergen (like eating peanuts or getting stung) and then develops any of these symptoms, treat it like anaphylaxis-even if you’re not 100% sure. Better to act fast than wait for confirmation.
Why Epinephrine Is the Only Treatment That Works
Antihistamines like Benadryl? They help with mild itching or a runny nose. But they do nothing to stop anaphylaxis. Steroids? They might reduce swelling later-but not in the moment. The only thing that can reverse anaphylaxis quickly is epinephrine.
Epinephrine works in two ways: it tightens blood vessels to raise blood pressure and opens up airways so you can breathe. It’s not a cure-it’s a life-preserving stopgap. Studies show that when epinephrine is given within minutes, 85% of patients improve within five minutes. If it’s delayed, that number drops to 42%.
Emergency rooms see this every day. A 2020 study found that more than half of patients who met the criteria for anaphylaxis didn’t get epinephrine at all. That’s not just a mistake-it’s a pattern. Too many doctors still reach for antihistamines first. But experts agree: epinephrine is the first and only step.
How to Use an Epinephrine Auto-Injector
Most people carry epinephrine in a pen-like device-EpiPen, Auvi-Q, or a generic version. These aren’t complicated, but most people don’t use them right.
Here’s how to do it:
- Remove the safety cap.
- Place the tip against the outer thigh-through clothing if needed.
- Push hard until you hear a click. Hold it in place for 3 seconds.
- Remove and massage the area for 10 seconds.
That’s it. No twisting. No fiddling. Just jab and hold. The injection goes into the muscle of the thigh, not under the skin. That’s because muscle absorption gets the drug into the bloodstream in 8 minutes-twice as fast as injecting into fat.
Many people freeze up. Needle fear affects nearly a quarter of users. That’s why practicing with a training device every month is critical. Keep one at home, in your car, at work, and at school. Don’t wait for a crisis to learn how to use it.

When to Give a Second Dose
One shot isn’t always enough. About 20% of anaphylaxis cases need a second dose. Symptoms might seem to improve after the first injection-then come back worse. That’s called a biphasic reaction, and it can happen hours later.
Guidelines say: if symptoms don’t improve-or get worse-after 5 minutes, give a second dose. Don’t wait. Don’t call 911 first. Don’t wait for an ambulance. Give the second shot, then call 911.
Emergency responders will give more epinephrine if needed, but you can’t wait for them. The clock starts the moment symptoms appear. Every minute counts.
What Not to Do
There are several dangerous myths about treating anaphylaxis:
- Don’t wait for a rash. No skin symptoms? Still anaphylaxis.
- Don’t give antihistamines first. They don’t stop airway swelling or shock.
- Don’t lie the person flat. If they’re having trouble breathing, sit them up. If they’re fainting, lie them down with legs raised.
- Don’t skip calling 911. Even if they feel better after epinephrine, they still need to go to the hospital. Biphasic reactions can strike 1 to 72 hours later.
One study found that 43% of people delay epinephrine because they think the symptoms aren’t bad enough. That’s the biggest reason people die from anaphylaxis.
Who Needs an Epinephrine Auto-Injector?
You don’t have to have had anaphylaxis before to need one. If you’ve had a serious allergic reaction-even once-you should carry epinephrine. So should anyone with:
- Known food allergies (especially peanuts, tree nuts, shellfish)
- History of insect sting reactions
- Severe asthma combined with any allergy
- Previous anaphylaxis from medication or latex
Doctors often prescribe epinephrine even if the reaction was mild-because the next one could be worse. The American Academy of Allergy, Asthma & Immunology says: if you’ve had one, you’re at risk for another.

Cost, Access, and Keeping Your Injector Ready
Epinephrine auto-injectors cost between $375 and $650 for a two-pack. That’s steep. But prices have dropped since generics entered the market-now covering 70% of prescriptions. Insurance helps, but many people still skip refills because of cost. One in three people can’t afford to replace expired pens.
Here’s how to stay prepared:
- Check the expiration date every month. Most pens last 12 to 18 months.
- Store at room temperature-no freezing, no leaving in a hot car.
- Use a reminder app to alert you when it’s time to replace.
- Keep one at home, one in your bag, one at work or school.
Schools in all 50 states now keep stock epinephrine for students without a personal device. That’s a big step forward. But only 37% of patients get a written emergency plan when they’re discharged from the hospital. That’s not enough.
New Options on the Horizon
In 2023, the FDA approved Neffy, a nasal spray version of epinephrine. It’s needle-free, easier for kids and needle-phobic adults, and works just as fast. It’s not a replacement for injectors yet-it’s an alternative.
Other innovations are coming: pens with Bluetooth that alert your emergency contacts, longer-lasting formulations, and apps that track exposure and symptoms. But none of these replace the core rule: epinephrine first, fast, and every time.
Final Takeaway: Act Immediately
Anaphylaxis doesn’t give you time to think. It doesn’t wait for a doctor. It doesn’t care if you’re scared of needles or if your pen expired last month. The only thing that matters is whether you act in the first five minutes.
If you or someone you love has a severe allergy, make sure you have epinephrine. Know how to use it. Practice with the trainer. Keep it with you. And never, ever wait for symptoms to get worse before giving it.
One dose can mean the difference between life and death. You don’t need to be a doctor to save a life. You just need to be ready.
Can antihistamines treat anaphylaxis?
No. Antihistamines like Benadryl may help with mild allergy symptoms like itching or hives, but they do nothing to stop the life-threatening airway swelling or drop in blood pressure that defines anaphylaxis. Using them instead of epinephrine delays proper treatment and increases the risk of death.
Where should I inject epinephrine?
Inject epinephrine into the outer thigh-through clothing if needed. This is the vastus lateralis muscle, which absorbs the drug fastest. Avoid injecting into the arm, buttocks, or fingers. The thigh is the only recommended site for auto-injectors.
Do I still need to call 911 after using epinephrine?
Yes. Even if symptoms improve, you must call 911 and go to the hospital. Anaphylaxis can have a delayed second wave (biphasic reaction) that happens hours later. Emergency care is required to monitor for complications and provide additional treatment if needed.
How often should I replace my epinephrine auto-injector?
Replace your auto-injector every 12 to 18 months, or sooner if the liquid inside turns brown or cloudy. Check the expiration date monthly. Many people delay refills due to cost, but using an expired pen is risky-it may not work when you need it most.
Can children use epinephrine auto-injectors?
Yes. Children weighing at least 15 kg (33 pounds) can use the 0.15 mg dose. For those over 30 kg (66 pounds), the adult dose (0.3 mg) is recommended. Training devices are available for practice. Schools and caregivers should be trained to administer epinephrine if a child has a reaction.









So let me get this straight-we’re telling people to jab themselves with a needle in the thigh during a panic attack, but we’re not teaching them how to do it until it’s too late? I mean, I get it, epinephrine saves lives, but if your life depends on your ability to follow a 4-step instruction while your throat is closing, we’ve already lost.
Why aren’t we automating this? Why isn’t every school, airport, and grocery store equipped with a smart auto-injector that calls 911, texts your emergency contacts, and administers the dose via AI-guided robotic arm? We have self-driving cars and AI that writes poetry-why can’t we have a device that doesn’t require human competence in a crisis?
Also, I’m 52 and I still freeze when I see a syringe. I’m not weak-I’m biologically programmed to avoid sharp things. The fact that we blame people for not using it instead of redesigning the system is frankly criminal.
And yes, I’ve had my EpiPen since 2018. It’s expired. I haven’t replaced it because the co-pay is more than my monthly Netflix subscription. This isn’t negligence. This is capitalism.
okay so i read this whole thing and like wow this is so important but also kinda terrifying?? like i have a cousin who is allergic to peanuts and she once had a reaction at a birthday party and everyone was like oh maybe its just a rash or she ate something weird and she almost died and i was like WHAT??
but also why do we even have to rely on people remembering 4 steps when theyre panicking?? like why isnt there a pill or a spray or something that just works without the whole needle thing?? i mean i get epinephrine is the only thing that works but why cant we make it easier??
also i saw this video where a kid used an epipen on his dad and the dad was like crying and saying thank you and i was like okay thats the kind of thing that makes me believe in humanity again
but also why is it so expensive?? like its a lifesaver and its like 600 bucks?? who even has that kind of money?? i think we need a universal epipen fund or something
also i think we should make epipen training mandatory in high school like sex ed but for not dying lol
😭 I used my EpiPen last year. Twice. First time: I thought it was a panic attack. Second time: I thought it was a bad burrito.
Turns out? Both times? Peanut dust on a bus seat. 🤦♂️
Now I carry two. One in my pocket. One taped to my inner thigh with duct tape. Just in case I pass out. Or forget. Or someone tries to take it from me thinking it’s a vape.
Also, I cried during the part about the nasal spray. I’m not ashamed. I’m a grown man. And I hate needles. 🤕💉
Also, the guy who said ‘don’t wait for a rash’? That’s me. I had a 20-minute silent anaphylaxis. No hives. Just wheezing. Like a dying teakettle. No one knew. I almost died. Because I thought I was just having asthma. 😭
Epinephrine isn’t a treatment. It’s a second chance. And I’m not letting mine expire.
Just want to say this is the most important thing i’ve read all year. I work at a school and we just got our stock epipens last month. We trained the staff. Now we’re teaching kids how to use them on each other. No drama. No fear. Just practice.
One 8-year-old girl told me, ‘I’m not scared of needles anymore. I’m scared of not being ready.’
That’s the future right there.
Also-yes, the cost sucks. But if your insurance won’t cover it, call the manufacturer. They have coupons. They have programs. You just have to ask.
And yes, check the expiration date. Every month. Set a reminder. Your life depends on it. Not ‘maybe.’ Not ‘if you’re lucky.’ Every. Single. Month.
I’ve been a nurse for 18 years and I still see people give Benadryl first. It breaks my heart. You’re not being cautious-you’re being dangerous.
My sister had anaphylaxis from a wasp sting. She didn’t have a rash. Just dizziness and nausea. She took an antihistamine. Waited 40 minutes. Then collapsed. By the time they got her to the hospital, her blood pressure was 60/30.
She’s fine now. But she carries two pens. And she makes everyone in her family practice on oranges. We have a whole ritual now. ‘Orange jab day.’ It’s weird. But it works.
Also-yes, the cost is insane. But if you can’t afford it, ask for samples. Ask for help. Don’t wait until it’s too late. I’ve seen too many people die because they thought ‘it won’t happen again.’
It will.
And you won’t get a second warning.
So let me get this straight-people are dying because they’re too lazy to carry a $600 pen? And now we’re supposed to feel bad for them?
My dog has a better survival plan than half the people I know.
You think your life is too busy to check an expiration date? Then maybe you shouldn’t be allowed near food. Or bees. Or anything that could possibly kill you.
Epinephrine isn’t optional. It’s not a luxury. It’s a basic survival tool. Like a seatbelt. Like fire extinguishers. If you don’t have one, you’re not a victim-you’re just reckless.
And if you’re too scared to use it? Then don’t eat peanuts. Don’t go outside. Don’t live. Simple.
While the general sentiment of this article is laudable, the lack of nuance regarding biphasic reactions is concerning. The claim that ‘20% of cases require a second dose’ is statistically misleading without citing the source population-most studies indicate this figure varies from 8% to 22% depending on etiology, age, and route of exposure.
Additionally, the assertion that ‘epinephrine is the only treatment that works’ is technically accurate but semantically reductive. Epinephrine is the only *immediate* pharmacologic intervention that reverses hemodynamic collapse; however, adjunctive therapies such as IV fluids, bronchodilators, and corticosteroids are essential for sustained recovery.
Furthermore, the omission of the fact that epinephrine auto-injectors have a 15–20% failure rate due to improper technique or device malfunction is a dangerous oversight. The article reads like a public service announcement written by a marketing team-not a clinical guideline.
And yes, I am a board-certified allergist. You’re welcome.
I’m from India and I just flew back to the U.S. last month. I was terrified. I have a child with a peanut allergy. In India, no one knows what an EpiPen is. I had to carry my own from home. I had to explain it to my in-laws. I had to translate the instructions into Hindi.
But here’s what changed me: at the airport, a stranger saw me holding the pen and asked, ‘Is that for your kid?’ I said yes. She pulled out her own. Said her son had one too. We sat there for 20 minutes, sharing stories. No words. Just nods. Just understanding.
That’s the thing nobody talks about. This isn’t just about medicine. It’s about community. It’s about not being alone in your fear.
So if you have a pen-carry it. If you don’t-get one. And if you see someone holding one? Don’t ask. Don’t judge. Just say, ‘I’ve got your back.’
Because sometimes, the most powerful medicine isn’t in the pen.
It’s in the person beside you.