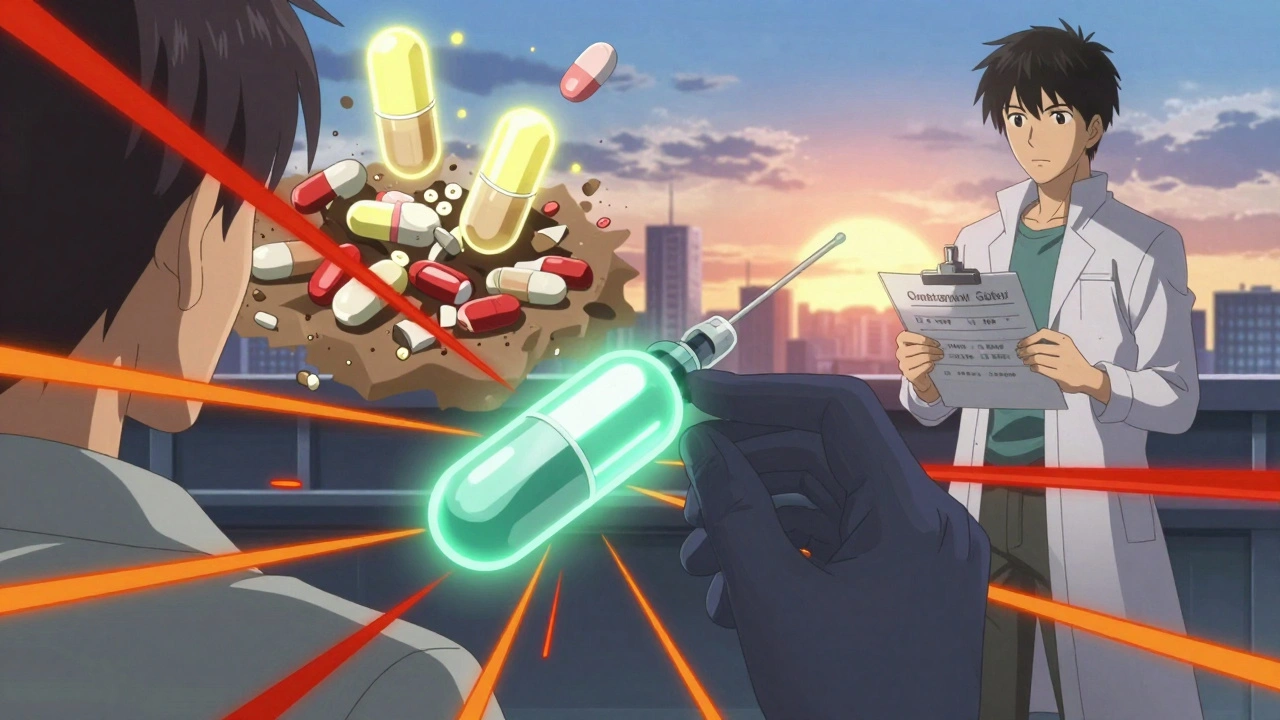
HIV Medication Interaction Checker
Check Your Medication Safety
This tool helps you identify potentially dangerous interactions between your HIV medications and common prescriptions, over-the-counter drugs, or supplements. Always consult your healthcare provider for personalized advice.
Interaction Results
When you're on antiretroviral therapy (ART) for HIV, taking the right pills at the right time isn't enough. Many of the everyday medications you might be using - for cholesterol, blood pressure, depression, or even a stuffy nose - can dangerously clash with your HIV drugs. These aren't theoretical risks. They're real, life-threatening interactions that happen more often than most people realize.
Why This Matters More Than Ever
About half of all people living with HIV in the U.S. are now over 50. That means more heart disease, more diabetes, more joint pain - and more pills. The average 65-year-old with HIV takes nearly 10 medications. Each one adds risk. In fact, every extra pill increases your chance of a dangerous interaction by 18%. And it’s not just prescriptions. Over-the-counter painkillers, herbal supplements like St. John’s Wort, and even recreational drugs can turn a stable treatment plan into a medical emergency.The Big Three: Which ART Drugs Cause the Most Problems?
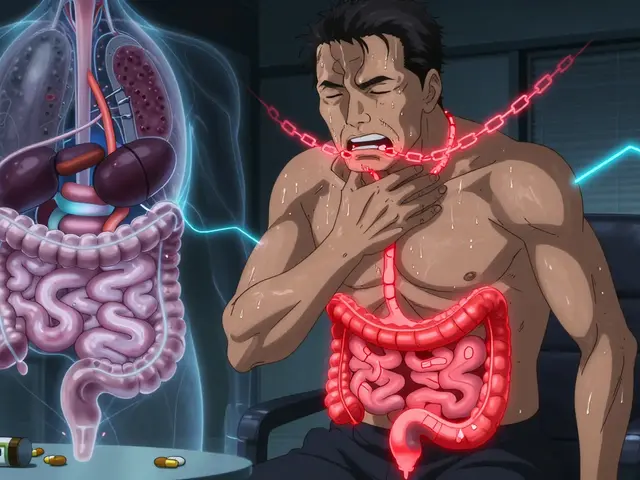
Not all HIV medications are created equal when it comes to drug interactions. The risk depends almost entirely on which class you’re taking.Protease inhibitors (PIs) boosted with ritonavir or cobicistat are the biggest offenders. These drugs block the liver’s CYP3A4 enzyme - the same system that breaks down more than half of all prescription medications. The result? Other drugs build up to toxic levels in your blood. Ritonavir alone has over 200 known interactions. Cobicistat isn’t much better.
Non-nucleoside reverse transcriptase inhibitors (NNRTIs) like efavirenz do the opposite: they speed up how fast your body clears other drugs. That means your blood pressure pills, antidepressants, or birth control might not work at all. Efavirenz cuts the levels of many medications by up to 75%. Etravirine and rilpivirine are safer, but still carry risks.
Integrase strand transfer inhibitors (INSTIs) - like dolutegravir and bictegravir - are the new gold standard. They barely touch liver enzymes. Bictegravir has only seven major interactions. Dolutegravir has about eight. That’s why most new patients start on these today. But even they aren’t perfect. Dolutegravir lowers metformin levels by 33%, which can mess with blood sugar control in people with diabetes.
Top 5 Deadly Interactions You Must Avoid
1. Statins + Boosted PIs = Rhabdomyolysis
Simvastatin and lovastatin are absolutely forbidden with ritonavir or cobicistat. These statins can spike in your blood by 20 to 30 times. That causes muscle breakdown - rhabdomyolysis - which can lead to kidney failure and death. Pitavastatin and fluvastatin are safe alternatives. Atorvastatin is okay in low doses. Rosuvastatin? Use with caution.
2. Inhaled Steroids + Boosted PIs = Adrenal Crisis
Fluticasone (Flovent), budesonide (Pulmicort), and even nasal sprays can cause Cushing’s syndrome or adrenal insufficiency when taken with boosted PIs. Your body stops making its own cortisol. You might feel weak, dizzy, or collapse from low blood pressure. A 2023 study found 17% of patients on these combos ended up hospitalized. Switch to beclomethasone or non-steroid inhalers if possible.
3. Erectile Dysfunction Drugs + Boosted PIs = Dangerous Overdose
Avanafil (Stendra) is completely off-limits. Sildenafil (Viagra) and tadalafil (Cialis) can be used - but only at reduced doses. With ritonavir or cobicistat, you can’t take more than 25mg of sildenafil every 48 hours. Normal doses can cause severe low blood pressure, fainting, or heart attack.
4. SSRIs + Boosted PIs = Serotonin Syndrome
Fluoxetine (Prozac), paroxetine, and sertraline can pile up with ritonavir. That leads to serotonin syndrome: high fever, confusion, fast heartbeat, muscle rigidity. It’s rare but deadly. If you’re on both, your doctor may need to cut your SSRI dose in half. Avoid fluoxetine entirely if you can - it’s the worst offender.
5. Rifampin + Bictegravir = Treatment Failure
Rifampin (used for TB or certain infections) slashes bictegravir levels by 71%. That means your HIV virus can start replicating again. You’ll need a different TB treatment or a switch to another INSTI like dolutegravir. Don’t assume all INSTIs are safe - this one’s a trap.
What About Herbal Supplements and Recreational Drugs?
St. John’s Wort is the most dangerous herbal supplement. It drops efavirenz levels by up to 60%. That’s enough to make your HIV treatment fail. Even garlic pills and grapefruit juice can interfere with some ART drugs. And recreational drugs? Ketamine, MDMA, and cocaine can stay in your system longer when you’re on ritonavir because your liver can’t process them. That means higher overdose risk, longer hallucinations, or heart problems.
How to Protect Yourself
There’s no magic bullet - but there are smart steps.
- Bring every pill, patch, and supplement to every doctor visit - even the ones you think don’t matter. That includes vitamins, CBD oil, and herbal teas.
- Use the Liverpool HIV Drug Interactions Checker. It’s free, updated monthly, and used by clinics worldwide. Type in your HIV meds and any new prescription - it tells you if it’s safe.
- Ask your pharmacist to run a drug interaction scan every time you fill a new prescription. Most pharmacies can do this automatically.
- Don’t stop or change doses on your own. If your doctor says to switch from a boosted PI to dolutegravir, your other meds (like tacrolimus or warfarin) will need dose changes. Too much or too little can be deadly.
- Get certified. The American Academy of HIV Medicine offers an 8-hour online course on drug interactions. Clinics that use it see 42% fewer bad reactions.
The Future Is Simpler
The good news? The next generation of HIV drugs is being designed to avoid these problems. Lenacapavir, injected twice a year, has almost no liver interactions - unless you’re also on rifampin. New drugs in development are being screened for interaction risk from day one. By 2030, the most common ART regimens are expected to have 80% fewer dangerous interactions than today’s boosted PIs.
For now, the safest path is clear: If you’re on a boosted PI, talk to your doctor about switching to an INSTI like dolutegravir or bictegravir - especially if you take multiple other meds. If you’re already on an INSTI, don’t assume you’re safe. Check every new drug before you take it. Your life depends on it.
Can I take ibuprofen with my HIV meds?
Yes, ibuprofen is generally safe with most antiretrovirals. Unlike NSAIDs like celecoxib or diclofenac, it doesn’t rely heavily on the CYP3A4 pathway. But if you’re on a boosted PI and have kidney issues or high blood pressure, talk to your doctor. Long-term use of any NSAID can strain your kidneys - and HIV already increases your risk for kidney disease.
Is it safe to take OTC cold medicine with ART?
Many cold medicines contain dextromethorphan, pseudoephedrine, or phenylephrine. Dextromethorphan can build up dangerously with boosted PIs and cause serotonin syndrome. Pseudoephedrine can raise blood pressure - risky if you’re also on a calcium channel blocker. Always pick single-ingredient products and check the Liverpool HIV Drug Interactions Checker before taking anything.
What if I’m on birth control and taking ART?
Efavirenz and some boosted PIs reduce the effectiveness of hormonal birth control. You could get pregnant even if you take your pill every day. Use a backup method like condoms or an IUD. If you’re on an INSTI like dolutegravir, hormonal birth control is usually fine - but still talk to your doctor. Some newer pills have lower estrogen, which might not be enough.
Can I take fish oil or vitamin D with HIV meds?
Yes. Fish oil and vitamin D have no known interactions with any antiretroviral drugs. In fact, many people with HIV are low in vitamin D, and fish oil helps reduce inflammation. These are safe supplements - but always tell your provider you’re taking them. Some brands add herbs or other ingredients that might cause problems.
I’m switching from a boosted PI to dolutegravir. What do I need to change?
When you stop ritonavir or cobicistat, your body starts processing other drugs faster again. Medications like tacrolimus, cyclosporine, or warfarin can drop to unsafe levels. Your doctor will likely reduce tacrolimus by 75%, cut warfarin doses, and monitor blood levels closely for weeks. Never switch ART without a plan for your other meds.
Are there any ART drugs that don’t interact with anything?
No drug is completely interaction-free. But dolutegravir and bictegravir come closest. They have only about 8 major interactions total. Lenacapavir, the new twice-yearly injection, has almost none - unless you’re on rifampin or certain seizure meds. The goal isn’t zero interactions - it’s minimizing them. INSTIs are the best choice for most people on multiple medications.
What to Do Next
If you’re on HIV treatment and take any other medications - even one - schedule a full med review with your doctor or pharmacist. Bring a list of everything: prescriptions, OTCs, supplements, and even occasional drugs like painkillers or sleep aids. Ask them to use the Liverpool HIV Drug Interactions Checker. If your provider doesn’t know how to use it, find one who does. There are free online tools and training courses available. Don’t wait for a crisis. The safest HIV treatment is the one that doesn’t clash with the rest of your life.







OMG. I just read this and I’m literally shaking. I’ve been on a boosted PI for 7 years and I’ve been taking ibuprofen like it’s candy. I just Googled ‘fluticasone + ritonavir’ and holy hell-I had no idea I was one bad sinus infection away from adrenal collapse. I’m calling my doctor tomorrow. Like, right now. This is life or death. I’m so mad I didn’t know this sooner.
fr fr if u r on ART and still takin st johns wort u aint tryna live. like bruh. i saw a guy on reddit last week say he took it with efavirenz and ended up in the er. he thought it was ‘natural’ so it was safe?? nah. natural doesn’t mean ‘not gonna kill u’. also grapefruit juice?? bro. just drink water.
While the article correctly identifies the CYP3A4-mediated interactions as the primary pharmacokinetic concern, it fails to adequately contextualize the clinical significance of these interactions relative to pharmacodynamic synergies. For instance, the risk of serotonin syndrome with SSRIs and boosted PIs is statistically elevated, yet the absolute incidence remains below 0.8% in prospective cohort studies. Moreover, the recommendation to avoid fluoxetine entirely is overly cautious-its long half-life actually mitigates peak concentration spikes, making it more predictable than sertraline in polypharmacy scenarios. The real issue is not the drug class, but the absence of therapeutic drug monitoring in routine HIV care. Without plasma concentration assays, we’re operating in the dark.
Man, I’ve been on dolutegravir for three years now and honestly, I thought I was in the clear. But reading this made me realize I’ve been ignoring my cholesterol meds like they’re optional. I’m on atorvastatin 10mg-didn’t even know that could be risky. I’ve got a stack of supplements I picked up from the health food store because ‘they’re good for immunity’. Guess what? I’m dumping them all tonight. Thanks for the wake-up call. This stuff matters. We all need to be better about this.
Let’s be real-this isn’t just about HIV meds. It’s about how broken our healthcare system is. Why is it on the patient to know that fluticasone + ritonavir = adrenal apocalypse? Why aren’t pharmacies flagging this automatically? Why does the Liverpool tool exist as a free, obscure website instead of being integrated into every EHR? This isn’t patient negligence. It’s systemic failure. And yet, we’re still blaming people for not being medical experts.
From a pharmacodynamic standpoint, the real paradigm shift is in INSTI dominance. The CYP3A4 avoidance profile of bictegravir and dolutegravir isn’t just ‘better’-it’s a quantum leap in polypharmacy safety. The 80% reduction in interaction burden projected by 2030 isn’t speculative; it’s already measurable in phase 4 trials. What’s more, the pharmacokinetic stability of lenacapavir (t½ >100 days) essentially decouples ART from hepatic metabolism. The future isn’t just safer-it’s simpler. We’re moving from daily pill burdens to biannual injections. This isn’t incremental progress. It’s transformational.
just wanted to say thank you for writing this. i’ve been on ART for 12 years and i never knew half this stuff. i thought my weird dizziness was just ‘aging’. turns out it was the fluticasone. i switched to beclomethasone last week and i feel like a new person 😊 also, i deleted st. john’s wort from my cart. no more ‘natural healing’ nonsense. real talk: this post saved my life. 🙏
There’s a quiet violence in how we normalize polypharmacy for people with chronic conditions. We hand out pills like candy-‘take this for blood pressure, this for cholesterol, this for sleep, this for anxiety’-and then act shocked when the system crashes. But we never ask: why do we treat HIV as an island? Why isn’t integrated care the default? Why is the burden of memorizing 200+ interactions placed on someone already managing a stigmatized illness? This isn’t just about drugs. It’s about dignity. We need care that meets us where we are-not a checklist that demands we become pharmacists.
As someone from India, where access to specialized HIV care is limited, this article is a lifeline. Many of us rely on generic ART and over-the-counter medications due to cost. The Liverpool tool is now bookmarked on my phone. I’ve shared it with my local clinic. We don’t have pharmacists who specialize in HIV, but we do have community health workers. They’re now trained to check interactions before dispensing any new drug. Small steps, but they matter. Thank you for making this accessible. Knowledge is power-and here, it’s survival.
My doctor switched me from boosted PI to dolutegravir last month. I didn’t realize my warfarin dose needed to change until I almost bled out. Now I have a blood test every week. I’m alive because I listened. If you’re on multiple meds-don’t wait for a crisis. Talk to your pharmacist. Use the tool. Ask again. And again. Your life is worth it.