Gallbladder Risk Assessment Tool
This tool helps you identify if you may be at risk for gallbladder issues while taking GLP-1 agonists like Ozempic or Wegovy. Based on your inputs, it will calculate your risk level and provide appropriate guidance.
Risk Assessment Form
Answer these questions to determine your risk level. This tool uses data from the JAMA Internal Medicine study showing increased gallbladder risk with GLP-1 agonists.
Risk Assessment Results
Your risk level and next steps:
When you start a GLP-1 agonist like Ozempic or Wegovy for weight loss or diabetes, the goal is clear: lose weight, improve blood sugar, feel better. But for some, a new kind of pain shows up - sharp, persistent, and often right under the ribs on the right side. This isn’t just indigestion. It could be your gallbladder screaming for attention.
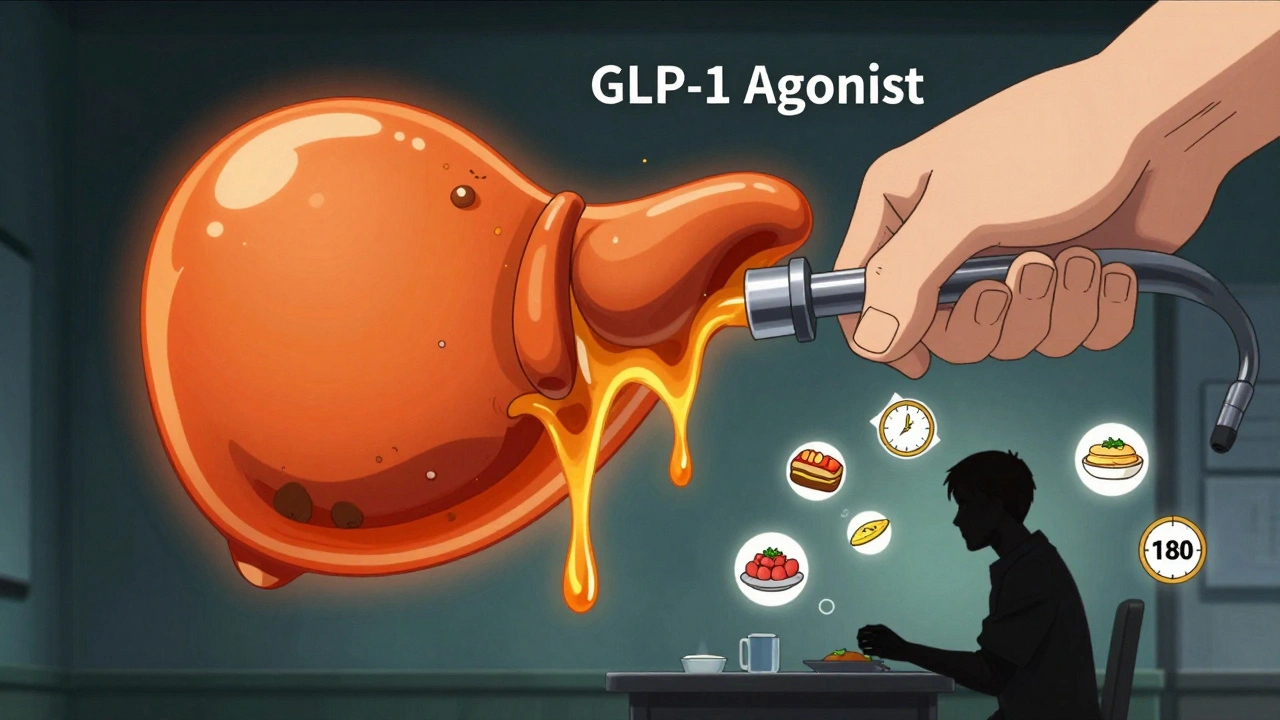
Why GLP-1 Agonists Put Your Gallbladder at Risk
GLP-1 agonists work by slowing down digestion. That’s why they help you feel full longer and lose weight. But that same effect hits your gallbladder hard. These drugs block a hormone called cholecystokinin, which tells your gallbladder to squeeze and release bile after you eat. Without that signal, bile sits there, thickens, and starts forming sludge - then stones. A major 2022 study in JAMA Internal Medicine looked at 56,000 people across 76 trials. The result? People on GLP-1 agonists had a 37% higher risk of gallbladder disease compared to those not taking them. That might sound small, but in real numbers, it means about 1 in 100 people on these drugs develop gallstones. For those using higher doses for weight loss - like Wegovy or Saxenda - the risk jumps even more. Liraglutide and semaglutide carry the highest risk. That’s not a coincidence. These are the drugs that cause the most weight loss - up to 15% of body weight. Rapid weight loss itself is a known trigger for gallstones. Combine that with the drug’s effect on bile flow, and you’ve got a perfect storm.What Abdominal Pain Looks Like When It’s Your Gallbladder
Not all belly pain is the same. If you’re on a GLP-1 agonist and feel pain, here’s how to tell if it’s something serious:- Location: Right upper quadrant (RUQ) - right under your ribs, sometimes radiating to your right shoulder or back.
- Timing: Starts 30 to 60 minutes after eating, especially fatty meals like pizza, fried chicken, or cheese.
- Duration: Lasts more than 30 minutes, often 1 to 5 hours. It doesn’t just go away with burping or antacids.
- Associated symptoms: Nausea, vomiting, fever, or dark urine. If you have all of these together, it’s a red flag.
When Does This Happen? Timing Matters
This isn’t something that happens on day two. Most cases show up after 3 to 9 months of treatment. The average time from starting the drug to gallbladder surgery is 180 days - right around six months. That’s why so many people think they’re fine: they’ve been on it for months without issues. Then, out of nowhere, the pain hits. And here’s the kicker: 93% of gallbladder problems linked to GLP-1 agonists happen within the first year. After that, the risk drops - but not to zero. If you’re still losing weight fast, your gallbladder is still under stress.Who’s Most at Risk?
Not everyone on these drugs will get gallstones. But some people are far more likely:- Women over 40
- People with a BMI over 30
- Those who’ve lost more than 1.5 kg (3.3 lbs) per week
- Anyone who’s had gallstones before - even if they were years ago
- People with type 2 diabetes (higher baseline risk)
What Happens If You Ignore the Pain?
Gallstones aren’t always an emergency. But when they block the bile duct or inflame the gallbladder (cholecystitis), things turn serious fast. About 75% of patients with GLP-1-related cholecystitis end up needing surgery to remove their gallbladder. That’s not minor. It’s a major operation with a recovery time of 4 to 6 weeks. And once your gallbladder is gone, you’re stuck with it. You can live without one, but your digestion changes forever. You might have more diarrhea, especially after fatty meals. You’ll need to adjust your diet long-term. The good news? If you catch it early, you might avoid surgery. Some doctors now recommend stopping the GLP-1 agonist and trying ursodeoxycholic acid (UDCA), a bile acid that can dissolve small stones. A clinical trial is currently testing this approach - early results look promising.What to Do If You Have Pain
Don’t wait. Don’t assume it’s just a stomach bug. If you’re on a GLP-1 agonist and feel this kind of pain:- Stop eating fatty foods immediately.
- Call your doctor - don’t wait for your next appointment.
- Ask for an abdominal ultrasound. This is the gold standard for spotting gallstones.
- Do NOT keep taking the drug until you know what’s causing the pain.
What About People Who’ve Already Had Their Gallbladder Removed?
If you’ve had a cholecystectomy, your risk of new gallstones is nearly zero. But there’s a small catch: leftover stones or sludge can still get stuck in the bile ducts. That’s rare, but possible. You’re not immune - just much safer. Still, if you feel new pain after starting a GLP-1 agonist, get it checked. Don’t assume it’s fine just because you’re “gallbladder-free.”
How This Compares to Other Weight Loss Drugs
Not all weight loss drugs carry this risk. Orlistat (Xenical) can cause oily stools and gas, but it doesn’t affect bile flow. Phentermine-topiramate has no known gallbladder risk. But GLP-1 agonists are unique in how deeply they interfere with digestion - and that’s why the gallbladder pays the price. The FDA updated the labels for all GLP-1 agonists in January 2023 to include gallbladder disease as a known risk. Semaglutide’s label now says 0.9% of users developed gallstones vs. 0.4% on placebo. That’s not huge - but it’s real, and it’s rising.The Bigger Picture: Why This Is Getting Worse
In 2021, there were fewer than 600 reports of gallbladder problems linked to GLP-1 drugs in the FDA’s database. In 2023? Over 1,800. That’s a 217% jump. Why? Because prescriptions have exploded. In 2021, about 1.2 million people used Wegovy. By late 2023, that number was over 6.8 million. More users = more cases. And here’s the quiet truth: many doctors still don’t know this link. A 2025 article in CCJM called it an “under-recognized risk in primary care.” Patients are often told, “It’s just side effects,” when it’s something serious. That’s why knowing the red flags is your best protection.What’s Next?
Researchers are already working on solutions. The Endocrine Society now recommends slower weight loss - no more than 1 kg (2.2 lbs) per week - for people at risk. Mayo Clinic is testing UDCA to prevent stones. And by 2026, experts predict all major drugmakers will include gallbladder risk checkers in their patient apps. For now, the message is simple: Know the signs. Act fast. Don’t ignore pain. Your gallbladder doesn’t warn you twice.Can GLP-1 agonists cause gallstones even if I’ve never had them before?
Yes. GLP-1 agonists slow gallbladder emptying, which can cause bile to thicken and form stones - even in people with no prior history. The risk is highest during the first 6 months of use, especially with rapid weight loss. Studies show about 1 in 100 people on these drugs develop gallstones, regardless of past history.
How soon after starting a GLP-1 drug do gallbladder symptoms usually appear?
Symptoms typically begin between 3 and 9 months after starting the medication. The average time to diagnosis or surgery is around 180 days. While rare cases occur earlier or later, over 90% of gallbladder issues linked to these drugs happen within the first year of use.
Is it safe to keep taking Ozempic or Wegovy if I have mild abdominal discomfort?
No. Mild discomfort can be an early sign of gallbladder inflammation. If you have right upper quadrant pain lasting more than 30 minutes, especially after eating fatty foods, stop the medication and get an ultrasound. Continuing to take the drug increases the risk of infection, blockage, or emergency surgery.
Do all GLP-1 agonists carry the same gallbladder risk?
No. Liraglutide and semaglutide carry the highest risk, especially at weight-loss doses (3.0 mg and 2.4 mg). Exenatide has a much lower risk. The difference is tied to how much weight loss the drug causes - and how strongly it suppresses gallbladder contractions. Higher doses = higher risk.
Should I get an ultrasound before starting a GLP-1 agonist?
If you’re a woman over 40, have a BMI over 30, are losing weight rapidly, or have a history of gallstones, yes. The American Association of Clinical Endocrinology recommends a baseline ultrasound for high-risk patients before starting treatment. It’s quick, non-invasive, and can prevent serious complications.
Can I still use GLP-1 agonists if I’ve had my gallbladder removed?
Yes - your risk of gallstones is nearly gone. But there’s still a small chance of bile duct blockage from leftover stones or sludge. If you develop new abdominal pain after starting the drug, get it checked. You’re not immune, but your risk is far lower than someone with a gallbladder.









I started Wegovy last year and had exactly this pain after pizza night. Thought it was just food poisoning. Ended up in the ER with gallstones. They removed my gallbladder. Don't ignore it. This post saved me from worse.
omg i thought i was just being dramatic but my right side has been killing me since feb... i was gonna keep taking ozempic till i saw this. gonna call my doc tmrw. thank u
I've been on semaglutide for 8 months and lost 32 lbs. No pain yet, but I'm getting an ultrasound next week just in case. My mom had gallbladder issues in her 50s, so I'm in the high-risk zone. Better safe than sorry. This is the kind of info we need more of.
This is why I love Reddit. Not every doc knows this. I'm a nurse and I've seen 3 patients in the last 6 months with this exact scenario. Stop the drug. Get the ultrasound. Don't wait for it to get worse. You can always restart later if it's clean.
It is not merely coincidental that the pharmaceutical industry's profit motive has led to the widespread prescription of GLP-1 agonists without adequate long-term safety data. The gallbladder is not a dispensable organ; its removal constitutes a permanent alteration of human physiology. One must question the ethical implications of promoting rapid weight loss at the cost of organ integrity.
I'm 42, BMI 34, on Wegovy for 5 months. Started having pain after a steak dinner. Called my endo right away. Got the ultrasound. Turns out it was sludge, not stones yet. They put me on UDCA and told me to cut fat. Pain went away in 3 days. I'm still on the drug, but now I eat like a rabbit. This info works.
The body remembers. Even when the mind is chasing numbers on a scale.
So let me get this straight - you're telling me I can't eat a cheeseburger without my gallbladder staging a coup? And I'm supposed to feel bad for this? I took a drug to lose weight, not to become a salad robot. If my body wants to revolt, let it revolt. I'll just eat less and cry into my kale.
Key point: the 37% relative risk increase translates to ~1% absolute risk - still low, but clinically significant in high-risk cohorts. Baseline USG is low-cost, high-yield. UDCA is off-label but biologically plausible. The real win is slowing weight loss to <1kg/week. That’s the modifiable variable most folks ignore. Also, remember: bile stasis + rapid adipose turnover = perfect storm. Not magic, just physics.
I appreciate the thoroughness of this post. It is imperative that patients and providers alike recognize the physiological consequences of pharmacologically induced metabolic shifts. The gallbladder is not an accessory organ; it is a vital component of lipid digestion. I recommend all prescribers integrate risk stratification into their clinical workflows before initiating therapy. Thank you for the evidence-based clarity.