INR Target Calculator
This tool helps you understand your target INR range based on your medical condition. Your target range depends on why you're taking warfarin.
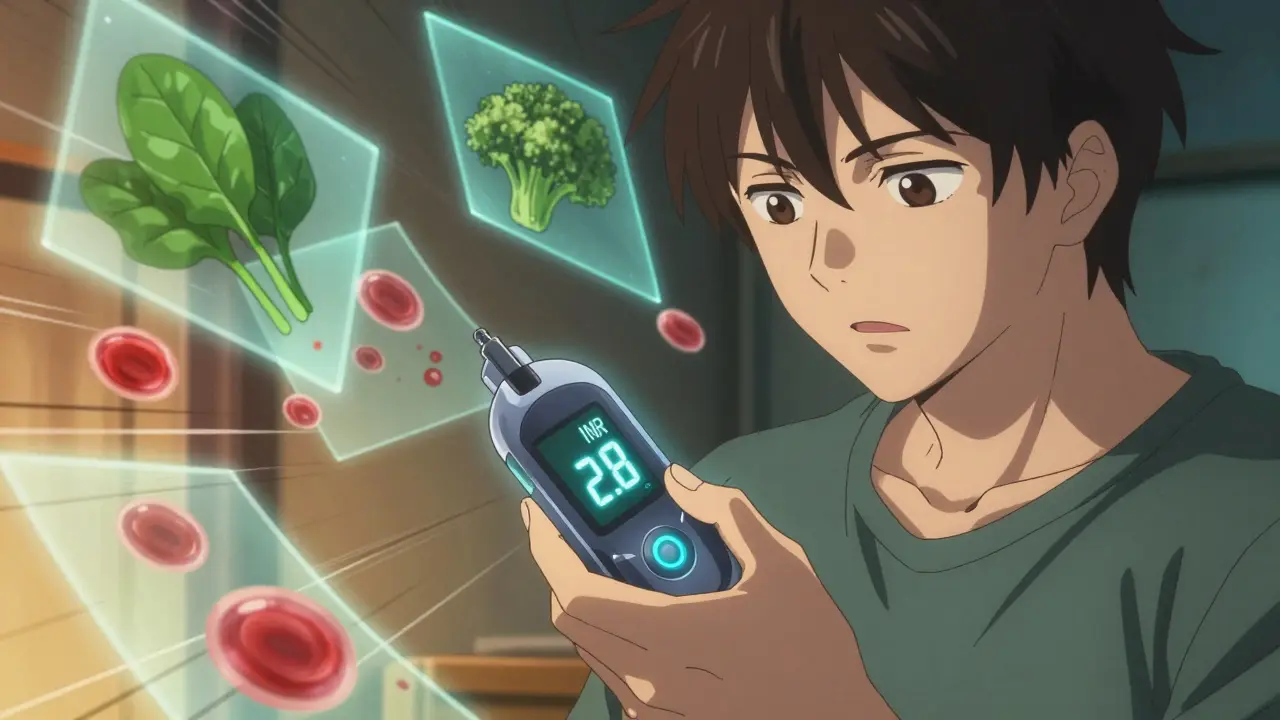
When you're on a blood thinner like warfarin, your life becomes a quiet dance with numbers. Not the kind you see on a scale or a fitness tracker, but a daily, sometimes hourly, awareness of something deeper: your INR. It’s not just a lab result. It’s a measure of how thin your blood is - and whether you’re safe from clots or at risk of bleeding. For millions of Americans, this number determines whether they can walk, drive, or sleep without fear. Understanding your INR isn’t optional. It’s survival.
What Exactly Is INR?
INR stands for International Normalized Ratio. It’s a standardized number that tells doctors how long it takes your blood to clot. The test starts with a simple blood draw or finger prick. The lab adds a substance that triggers clotting and times how long it takes. That raw time is called Prothrombin Time (PT). But here’s the catch: every lab uses slightly different chemicals. Without INR, a PT of 15 seconds in one hospital could mean something totally different than 15 seconds in another.
The INR fixes that. It’s a math formula that adjusts your PT based on the sensitivity of the reagent used. That way, an INR of 2.5 means the same thing whether you’re tested in Seattle, Atlanta, or a rural clinic in Montana. Before INR was standardized in 1983, patients on warfarin had unpredictable outcomes. Now, it’s the universal language of anticoagulation.
What’s the Right INR Range for You?
There’s no single perfect number. Your target INR depends on why you’re on a blood thinner.
- If you have atrial fibrillation or a blood clot in your leg or lung, your target is usually 2.0 to 3.0.
- If you have a mechanical heart valve - especially in the mitral position - you’ll likely need a higher range: 2.5 to 3.5.
- For a mechanical aortic valve, it’s typically 2.0 to 3.0, but your doctor may adjust it based on your age, valve type, or other conditions.
Going below 2.0 means your blood is clotting too fast. You’re at risk for stroke or another clot. Going above 3.0? You’re bleeding more easily. An INR over 4.9 doubles your risk of a major bleed. Each 0.5-point increase above 3.0 raises your bleeding risk by 27%. That’s not a small margin. It’s why precision matters.
Why Do You Need to Test So Often?
Warfarin doesn’t work like a pill you take and forget. It’s sensitive to diet, other meds, even your sleep schedule. A big bowl of kale can drop your INR. An antibiotic can spike it. A missed dose? That changes things too.
At first, you’ll test often - maybe twice a week. That’s when your doctor is finding your right dose. Once you’re stable, most people test once a month. But “stable” doesn’t mean “done.” Even if your INR has been perfect for six months, your body changes. Liver function, weight, hydration, stress - all of it affects warfarin.
Studies show that patients who test regularly and stay within their target range have 42% fewer strokes and 28% fewer major bleeds. That’s not luck. That’s consistency.

Home Testing: Is It Worth It?
For many, going to a lab every few weeks is a hassle. You take time off work. You wait in line. You get anxious waiting for results. Home INR testing changes that.
Devices like the Abbott Acelis or Roche CoaguChek let you prick your finger, drop a tiny drop of blood on a strip, and get a result in under a minute. No waiting. No phone calls. You know right away if your INR is off.
People who test at home spend 72% of their time in the target range. Those who go to clinics? Only 58%. That difference cuts stroke risk by 34% and major bleeding by 21%. It’s not just convenient - it’s life-saving.
But it’s not for everyone. If you have shaky hands, poor eyesight, or trouble remembering steps, home testing can be risky. About 25-30% of older adults or those with cognitive issues can’t manage it safely. And the devices aren’t cheap. The machine costs around $300. Each test strip is about $6. Medicare covers it fully for eligible patients. Private insurance often covers it too, but you might need a doctor’s note and fight a denial first.
Warfarin vs. Newer Blood Thinners
You might wonder: why not just switch to a newer drug like apixaban or rivaroxaban? They don’t need INR testing. You take them once or twice a day. No blood draws. No fuss.
That’s true - and that’s why they’re now the first choice for most people with atrial fibrillation. But here’s the catch: they don’t work for everyone.
- If you have a mechanical heart valve, warfarin is still the only option.
- If you have severe kidney disease, some newer drugs aren’t safe.
- Warfarin costs about $4 a month. The newer drugs? $550 to $650.
So while DOACs (direct oral anticoagulants) are growing fast - they’ll make up 85% of new starts by 2028 - warfarin still has a critical place. About 3.2 million Americans still rely on it. And for them, INR monitoring isn’t a burden. It’s the only thing keeping them alive.
What to Do If Your INR Is Too High or Too Low
Let’s say you test at home and your INR is 1.2. That’s too low. You’re at risk for a clot. Call your doctor. Don’t double your dose yourself. That’s dangerous. Your doctor might tell you to take an extra pill or two over the next few days - or they might suggest a different approach.
If your INR is 5.5? That’s dangerous. You’re bleeding internally without knowing it. Stop taking warfarin. Call your doctor immediately. If you’re dizzy, bruising easily, or have blood in your urine or stool, go to the ER. INR above 5.0 is an emergency.
And don’t ignore the small things. A cold, a new supplement, even a change in your vitamin K intake (found in spinach, broccoli, Brussels sprouts) can swing your INR. Keep a log. Write down what you eat, what meds you take, how you feel. Bring it to every appointment.

How to Stay on Track
Staying in range isn’t about perfection. It’s about awareness. Here’s what works:
- Test at the same time every day - ideally between 8 a.m. and noon, after fasting for 4 to 6 hours.
- Keep your vitamin K intake steady. Don’t suddenly eat a lot of greens one week and none the next.
- Use a reminder app or calendar. Missed tests are the #1 reason INR goes out of range.
- Know your numbers. Don’t let your doctor be the only one who knows your INR.
- If you’re on home testing, make sure you’re trained properly. Two to four supervised sessions are standard. Don’t skip them.
And remember: your INR isn’t a score. It’s a signal. A quiet, steady, life-saving signal.
What’s Changing in 2025?
Technology is catching up. In early 2023, the FDA approved the first smartphone-connected INR monitor. You prick your finger, the device syncs to your phone, and your doctor gets the result automatically. No calls. No faxes. Just data.
Some clinics are now using AI tools to predict your next warfarin dose. One system from Mayo Clinic got it right 83% of the time. That’s better than most humans.
But the biggest challenge isn’t tech - it’s access. In rural areas, only 35% of clinics offer full anticoagulation management. In cities? 82%. That gap means people in small towns are more likely to have strokes because they can’t get tested often enough.
And while newer drugs are taking over, warfarin still saves lives. For those who need it, INR monitoring isn’t outdated. It’s essential.
What is a normal INR if I’m not on blood thinners?
If you’re not taking any anticoagulants, your normal INR is 1.0. This means your blood clots at the expected rate. Any number above 1.0 indicates your blood is taking longer to clot, which is intentional when you’re on warfarin. A result below 1.0 is rare and usually means a lab error or a problem with the test sample.
Can I check my INR at home?
Yes, if you’re on warfarin and your doctor approves it. Home INR monitors like the Abbott Acelis or Roche CoaguChek use a small drop of blood from your finger and give results in under a minute. These devices are FDA-approved and covered by Medicare and most private insurers for eligible patients. You’ll need training to use them safely and accurately.
How often should I test my INR?
When you first start warfarin, you’ll test every few days to find your right dose. Once stable, most people test once a month. Some may need testing twice a week if their INR is unstable, if they’re sick, or if they start a new medication. If you’re on home testing, you may test more often - but always follow your doctor’s plan. Testing too often without cause can lead to unnecessary dose changes and more risk.
What happens if my INR is too high?
An INR above 4.9 puts you at high risk for serious bleeding - even from minor injuries. If your INR is above 5.0, you should stop taking warfarin immediately and contact your doctor. If you have signs of bleeding - unusual bruising, blood in urine or stool, severe headaches, dizziness - go to the emergency room. Your doctor may give you vitamin K or fresh frozen plasma to reverse the effect quickly.
Can I eat leafy greens while on warfarin?
Yes - but keep your intake consistent. Leafy greens like spinach, kale, and broccoli are high in vitamin K, which counteracts warfarin. Eating a lot one week and almost none the next will make your INR swing wildly. You don’t need to avoid them. Just eat about the same amount every day. A consistent diet helps your INR stay stable.
Are newer blood thinners better than warfarin?
For many people, yes - they don’t need INR monitoring and have fewer food and drug interactions. But they’re not for everyone. If you have a mechanical heart valve, severe kidney disease, or can’t afford the high cost, warfarin is still the best option. The choice depends on your condition, lifestyle, and budget. Talk to your doctor - don’t switch on your own.
What Comes Next?
If you’re just starting on warfarin, expect a learning curve. It’s not about memorizing numbers. It’s about building habits. Test on time. Eat consistently. Track your meds. Know your warning signs.
If you’ve been on it for years, don’t get complacent. Your body changes. Your life changes. So should your monitoring.
And if you’re thinking about switching to a newer drug - ask your doctor if it’s right for you. But if you’re one of the 200,000 Americans with a mechanical valve, know this: your INR isn’t a burden. It’s your shield. And keeping it in range? That’s how you keep living.









Man, this post hit home. I’ve been on warfarin for six years now with a mechanical mitral valve. My INR’s been stubbornly hovering around 2.8 for months, and I swear my kale smoothies are the only thing keeping me alive. Consistency is everything - not perfection. Just show up, test, eat the same damn greens every day, and don’t panic over a 0.3 swing.
As someone who works in rural healthcare, I see the gap every day. In our clinic, we have patients driving two hours for a single INR test. Home monitors are life-changing - if they can afford them and have the dexterity. But insurance denials? Still a nightmare. We need better access, not just better tech.
i just started warfarin last month and honestly i had no idea how much goes into this like i thought it was just take pill and go but wow the diet the timing the logs its a full time job lol
Everyone acts like INR monitoring is some sacred ritual. Newsflash: most people on warfarin are just lucky they didn’t bleed out yet. The whole system is outdated. Switch to DOACs already. If you can’t afford it, that’s not your fault - it’s the system’s. Stop romanticizing outdated medicine.
lol i think this is all too much stress 😅 my cousin in india takes pills and never checks anything… he’s 72 and still rides his scooter daily 🤷♂️ maybe we overthink this? 🌿
Just came back from Nigeria where I’m volunteering - we don’t have INR machines, but we have community health workers who walk door to door with portable devices. It’s not perfect, but it’s working. This isn’t just about tech - it’s about human connection. Someone checking in on you? That’s the real magic.
bro i had an INR of 6.1 last year and i thought i was gonna die… turned out i just ate a whole bag of spinach after a 3-day fast 🤡 now i keep a food diary like it’s my bible. warfarin don’t play. i’m alive because i listened. no cap.
It’s funny how something so small - a leaf of spinach, a missed test, a good night’s sleep - can mean the difference between life and a hospital bed. We treat INR like a number, but it’s really a rhythm. A quiet, daily act of care. You don’t have to be perfect. Just present. That’s enough.