When doctors prescribe prednisone or prednisolone, it’s usually because something in your body is raging out of control-your immune system attacking your joints, your lungs swelling from an allergic reaction, or your intestines inflamed from Crohn’s disease. These drugs work fast. Really fast. But they come with a price tag written in side effects-some mild and temporary, others serious and lasting. If you’ve been told to take one of these steroids, you’re not alone. Over 12 million Americans get them every year. But knowing what to expect isn’t just helpful-it’s necessary to stay safe.
How Prednisone and Prednisolone Are Different (And Why It Matters)
Prednisone and prednisolone are almost twins in how they work, but there’s one big difference: your liver. Prednisone is a prodrug. That means your body has to turn it into prednisolone before it can do anything. If your liver is healthy, this happens smoothly. If it’s not-say, from cirrhosis or hepatitis-your body struggles to convert it. In those cases, doctors skip prednisone entirely and give you prednisolone directly. It’s like giving someone a key to unlock a door versus giving them the already-unlocked door. One requires effort. The other doesn’t.For most people, 5 mg of prednisone equals 5 mg of prednisolone in effect. But if your liver is damaged, that 5 mg of prednisone might as well be 2 mg. That’s why switching medications isn’t just about brand names-it’s about your biology.
Short-Term Side Effects: What Happens in the First Few Weeks
Most people start feeling the effects of these drugs within hours. The inflammation fades. The pain eases. But so does your sense of normalcy.- Insomnia hits nearly 7 out of 10 people. It’s not just trouble falling asleep-it’s being wide awake at 3 a.m. with your brain racing. Taking your dose before 2 p.m. cuts this risk in half.
- Increased appetite is almost universal. You’re not lazy-you’re wired. Your body thinks it’s in survival mode and wants to store energy. That’s why people gain 5 to 15 pounds in just a few weeks, even if they eat the same.
- Mood swings are real. Some feel euphoric. Others get irritable, anxious, or even paranoid. One Reddit user described calling 911 because he thought spiders were crawling on his walls-when there were none. At doses above 40 mg daily, this isn’t rare.
- Fluid retention causes swelling in your ankles, face, and hands. Your clothes feel tighter. Your rings won’t come off. This isn’t just water weight-it’s sodium pulling fluid into tissues, raising your blood pressure too.
- Headaches, dizziness, and sweating are common. You might feel like you’re coming down with the flu, but you’re not sick-you’re just reacting to the drug.
These symptoms aren’t signs you’re doing something wrong. They’re signs the drug is working. Most fade within two weeks of stopping. But that doesn’t mean you should quit cold turkey. More on that later.
Long-Term Side Effects: The Hidden Costs
If you’re on these drugs for more than three months, the risks shift from annoying to dangerous.- Bone loss is the silent thief. Every year you’re on more than 5 mg daily, your bone density drops. After two years, over 60% of long-term users develop osteoporosis. Broken hips and spine fractures become real threats. Walking isn’t enough-you need weight-bearing exercise and calcium plus vitamin D supplements.
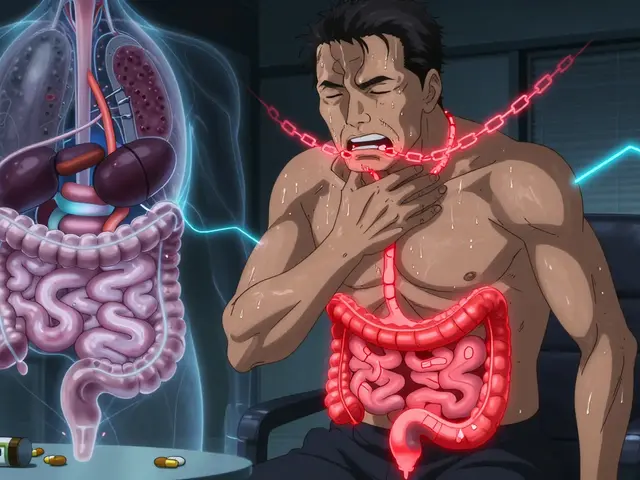
- Diabetes can appear out of nowhere. Even if you’ve never had high blood sugar, prednisone makes your liver pump out glucose and your body ignore insulin. Over half of non-diabetics on 20 mg or more develop steroid-induced diabetes. Monitoring your blood sugar isn’t optional-it’s life-saving.
- Cataracts and glaucoma creep up slowly. After years of use, 40% of patients need cataract surgery. Eye pressure rises, damaging the optic nerve. Annual eye exams aren’t a luxury-they’re mandatory.
- Adrenal suppression is the most dangerous. Your body stops making its own cortisol because the drug is doing it for you. If you stop suddenly, your body can’t snap back. You could go into adrenal crisis-low blood pressure, vomiting, confusion, even death. That’s why you must taper off slowly, over weeks or months, no matter how good you feel.
- Weight gain and "moon face" are visible, and they hurt. The round, puffy face, thickened neck, and belly fat aren’t just cosmetic. They’re signs your metabolism is stuck in overdrive. For kids, this can stunt growth by over an inch per year at higher doses.
- Wound healing slows. A simple cut takes longer to close. Surgery becomes riskier. Skin bruises easily. You might not notice until you get a scrape and it doesn’t heal for weeks.
These aren’t rare outcomes. They’re predictable. And they’re preventable-with the right plan.

Who Gets Hit Hardest? Age, Dose, and Duration Matter
Not everyone reacts the same. Risk climbs with three things: higher dose, longer time, and older age.Dr. Robert Kimberly says the danger spikes above 7.5 mg daily for more than three weeks. At 20 mg daily for eight weeks, nearly 4 in 10 people get a major side effect. For children, even low doses can slow growth. For seniors, bone fractures and infections become deadly.
Women are more likely to develop osteoporosis. Diabetics see blood sugar spiral. People with high blood pressure get worse. And if you’ve had stomach ulcers before? Prednisone can bring them back-hard.
There’s no magic number where side effects start. But the longer you’re on it, the more your body pays the price.
How to Manage the Side Effects-Without Stopping the Drug
You don’t have to suffer through this blindly. There are proven ways to reduce damage while still getting the benefits.- Take it early. Taking your dose before 2 p.m. reduces insomnia by almost 60%. Your body’s natural cortisol rhythm gets less disrupted.
- Watch your salt. Limit sodium to under 2,000 mg a day. Eat more potassium-rich foods-bananas, spinach, sweet potatoes-to balance fluid levels and protect your heart.
- Protect your bones. Get a bone density scan if you’re on more than 5 mg daily for over three months. Take calcium (1,200 mg) and vitamin D (800-1,000 IU) daily. Walk or lift weights three times a week.
- Guard your stomach. If you’re on more than 5 mg daily for over four weeks, your doctor should give you a proton pump inhibitor like omeprazole. It cuts ulcer risk from 8% to under 2%.
- Check your eyes. Annual eye exams catch glaucoma and cataracts early. Don’t wait for blurry vision.
- Monitor blood sugar. If you’re on 20 mg or more, test your glucose at least once a week. If it’s rising, your doctor might need to adjust your diet or add medication.
- Never skip or double doses. Missing a dose can trigger adrenal crisis. Doubling up can cause toxicity. Use a pill organizer or app-studies show they improve adherence by 37%.
These aren’t suggestions. They’re survival tactics.
When Prednisolone Might Be Better Than Prednisone
For most people, it doesn’t matter. But in three cases, prednisolone wins:- Liver disease. If your liver can’t convert prednisone, prednisolone is the only option.
- Children with IBD. Pediatric gastroenterologists prefer prednisolone for inflammatory bowel disease in kids-63% of them use it.
- Severe nausea. Prednisolone comes in liquid and orally disintegrating tablets (like Orapred ODT), which are easier to swallow if you’re feeling sick.
Otherwise, the choice often comes down to cost and availability. Generic prednisone is cheaper and easier to find. But if your body can’t process it, price doesn’t matter.

What Happens When You Stop?
This is where most people mess up. They feel better. They stop. And then they crash.Stopping suddenly can cause adrenal insufficiency-your body can’t make cortisol fast enough. Symptoms: extreme fatigue, dizziness, nausea, low blood pressure, even coma. That’s why tapering isn’t optional. It’s life-or-death.
Most people need at least 2 to 4 weeks to taper. Some need months. Your doctor will give you a schedule. Stick to it. Even if you feel fine. Even if you think you’re strong enough to quit cold turkey. You’re not.
And after you stop? Your body needs time to wake up. It can take weeks or months for your adrenal glands to start making cortisol again. Don’t rush back into stress, illness, or physical strain. Give yourself space to recover.
The Bottom Line: Are They Worth It?
Yes. But only if you use them wisely.For acute flare-ups-like a bad asthma attack, severe allergic reaction, or sudden lupus flare-these drugs are miracles. The GiACTA trial showed 92% of patients with giant cell arteritis improved with prednisone versus 58% on placebo. That’s life-saving.
But for long-term control? That’s where the cost climbs. Biologics like tocilizumab now help reduce steroid use in rheumatoid arthritis by nearly a third. New drugs are in trials that promise the same anti-inflammatory power without the side effects.
Right now, prednisone and prednisolone are still the best tools we have for many conditions. But they’re not forever drugs. They’re bridge drugs. They buy you time-time for other treatments to kick in, time for your body to heal, time to get off them safely.
Use them like fire: powerful, fast, and dangerous if left uncontrolled. With the right plan, monitoring, and discipline, you can use them without losing your health.
Can prednisone or prednisolone cause weight gain even if I eat healthy?
Yes. These drugs change how your body stores fat and retains fluid. Even if you eat clean, you’ll likely gain weight-especially around your face, belly, and back of the neck. This isn’t about calories. It’s about hormones. The weight usually drops after you stop, but it can take weeks or months.
Is prednisolone safer than prednisone?
For people with healthy livers, no-they’re equally risky. But if you have liver disease, prednisolone is safer because your body doesn’t need to convert it. In children and people with nausea, prednisolone’s liquid or disintegrating tablet forms are easier to take, making it the preferred choice in those cases.
How long do side effects last after stopping?
Short-term effects like insomnia, appetite changes, and mood swings usually fade within 1-2 weeks. But long-term damage-like bone loss, cataracts, or adrenal suppression-can be permanent. That’s why tapering and monitoring are critical. Your body needs time to recover, and some changes never fully reverse.
Can I take prednisone if I have diabetes?
Yes, but with caution. Prednisone raises blood sugar, often dramatically. If you have diabetes, your doctor will likely adjust your insulin or oral meds. You’ll need to check your blood sugar more often-sometimes several times a day. Many people with diabetes can safely use short-term prednisone if their glucose is closely monitored.
Why do I need to take prednisone with food?
Taking it with food reduces stomach irritation and lowers the risk of ulcers. It doesn’t affect how well the drug works, but it helps protect your digestive system-especially important if you’re on it for more than a few weeks. Avoid spicy or acidic foods, which can make stomach upset worse.
Are there natural alternatives to prednisone?
No. There are no natural supplements or herbs that replicate the powerful anti-inflammatory effect of prednisone or prednisolone. While some, like turmeric or omega-3s, have mild anti-inflammatory properties, they can’t replace steroids in treating serious autoimmune or allergic conditions. Don’t trade your doctor’s prescription for a supplement without talking to them first.
Can prednisone cause permanent adrenal damage?
Yes. After long-term use (usually over 6 months at moderate to high doses), your adrenal glands can stop making cortisol permanently. This is called secondary adrenal insufficiency. You’ll need lifelong hydrocortisone replacement. That’s why tapering slowly and avoiding long-term use whenever possible is critical.
How often should I get blood tests while on prednisone?
If you’re on it for more than a month, expect blood tests every 4-6 weeks. These check your blood sugar, electrolytes (especially potassium), liver function, and bone health markers. For long-term users, bone density scans and eye exams are needed annually. Don’t skip these. They catch problems before they become emergencies.
What Comes Next?
If you’re on prednisone or prednisolone, your next step isn’t just about taking the pill. It’s about managing your health around it. Talk to your doctor about:- A tapering plan before you even start
- Getting a bone density scan if you’ll be on it over 3 months
- Starting calcium, vitamin D, and a PPI if you’re on more than 5 mg daily
- Setting up regular glucose and eye checks
- Exploring alternatives like biologics if you’re on it long-term
These drugs save lives. But they don’t come with a warranty. You have to be your own advocate. Track your symptoms. Ask questions. Don’t let fear stop you from taking them when you need them-but don’t let complacency let you ignore the risks.








I was on this for 6 weeks after my flare-up. Lost 10 lbs of muscle and gained 15 of water weight. Felt like a balloon. 😅 But hey, I could walk again, so I ain't complaining.
It's irresponsible to suggest people use these drugs without fully understanding the lifelong consequences. Many don't realize they're trading short-term relief for permanent damage.
YESSS! 🙌 I'm a nurse and I see this EVERY WEEK. People think 'it's just steroids' and then show up with a broken hip and blood sugar at 450. Take the calcium. Watch the salt. Get your eyes checked. Don't be that person. 💪🩺
Man, I didn't realize how much my mood swings were from the meds until I stopped. I went from laughing at everything to crying over spilled coffee. Weird stuff.
This country is falling apart when we have to rely on chemical crutches just to get through the day. We used to heal naturally. Now? Pop a pill and call it a day. Pathetic.
It is imperative that patients adhere to the prescribed tapering protocol, as abrupt discontinuation may precipitate an adrenal crisis, which constitutes a medical emergency requiring immediate intervention.
So like... prednisone is basically the villain origin story for your body? 😭 I went from running marathons to needing a cane because my bones turned to dust. And my face? Looked like a full moon. I’m not mad… just… devastated.
You got this. I know it feels like your body’s betraying you, but you're not weak for needing this. You're strong for sticking with it and learning how to manage it. One day at a time.
It's funny how we treat the body like a machine you can just tweak with chemicals. But it's alive. It remembers. It fights back. Prednisone doesn't fix the root-it just silences the scream. And silence isn't healing.
In India, many patients get prednisolone because it's cheaper and available without liver conversion issues. Also, liquid form helps kids who can't swallow pills. Good info.
Let me tell you something, dear reader-this is not a drug, it's a slow-motion suicide pact disguised as relief. You think you're getting better? You're just buying time on borrowed organs. Your liver, your bones, your pancreas-they're all counting the days until you collapse. And when you do, no one will say 'I told you so'... because they were too busy taking their own pills.
Oh please. You think this is bad? Try being on biologics for 8 years and paying $20,000 a month. At least prednisone is $4 at Walmart. You want magic? Go live in a cave and pray to the moon. This is medicine, not a spa day.
Steroid-induced hyperglycemia is mediated via gluconeogenesis upregulation and insulin resistance at the peripheral level. Monitoring fasting glucose and HbA1c is mandatory in chronic users. Additionally, DEXA scans should be initiated at 3 months if dose exceeds 7.5 mg/day.
I used to think steroids were the devil. Then my daughter got sick. We had no choice. She gained weight, lost her energy, cried every night. But she lived. And now? She's 12, off the meds, and running track. It's not the answer-it's the bridge. And bridges aren't meant to be lived on. They're meant to be crossed.