Antihistamine Side Effect Comparison Tool
Choose Your Antihistamine
Select the antihistamine you're taking or considering to see its side effect profile
Side Effect Comparison
Select your antihistamine to see side effect comparison
When you take an antihistamine for allergies, you’re probably thinking about sneezing, runny nose, or itchy eyes. But many people don’t realize that some of the most common antihistamines-especially the cheap, over-the-counter ones-can cause side effects that hit much harder than a stuffy nose. Dry mouth, constipation, and urinary issues aren’t just minor annoyances. They’re signs of something deeper: anticholinergic effects. These aren’t rare or unusual. They’re built into the chemistry of first-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and promethazine. And for millions of people, especially those over 65, these effects are turning everyday life into a daily struggle.
How Antihistamines Cause Anticholinergic Side Effects
Antihistamines work by blocking histamine, the chemical your body releases during allergic reactions. But first-generation antihistamines don’t stop there. They also block another key chemical in your body: acetylcholine. Acetylcholine is a neurotransmitter that helps control muscle contractions, gland secretions, and nerve signals. When antihistamines interfere with it, you get what’s called anticholinergic activity. This isn’t a bug-it’s a feature. These drugs were designed in the 1940s to cross the blood-brain barrier and cause drowsiness. That’s why they were used as sleep aids and motion sickness meds. But the same property that makes them sedating also causes trouble in your mouth, gut, and bladder. Think of it like this: acetylcholine is the key that turns on your salivary glands, bowel movements, and bladder contractions. Antihistamines like diphenhydramine jam that keyhole. No key, no function. And the result? Three very common-and very uncomfortable-side effects.Dry Mouth: More Than Just Uncomfortable
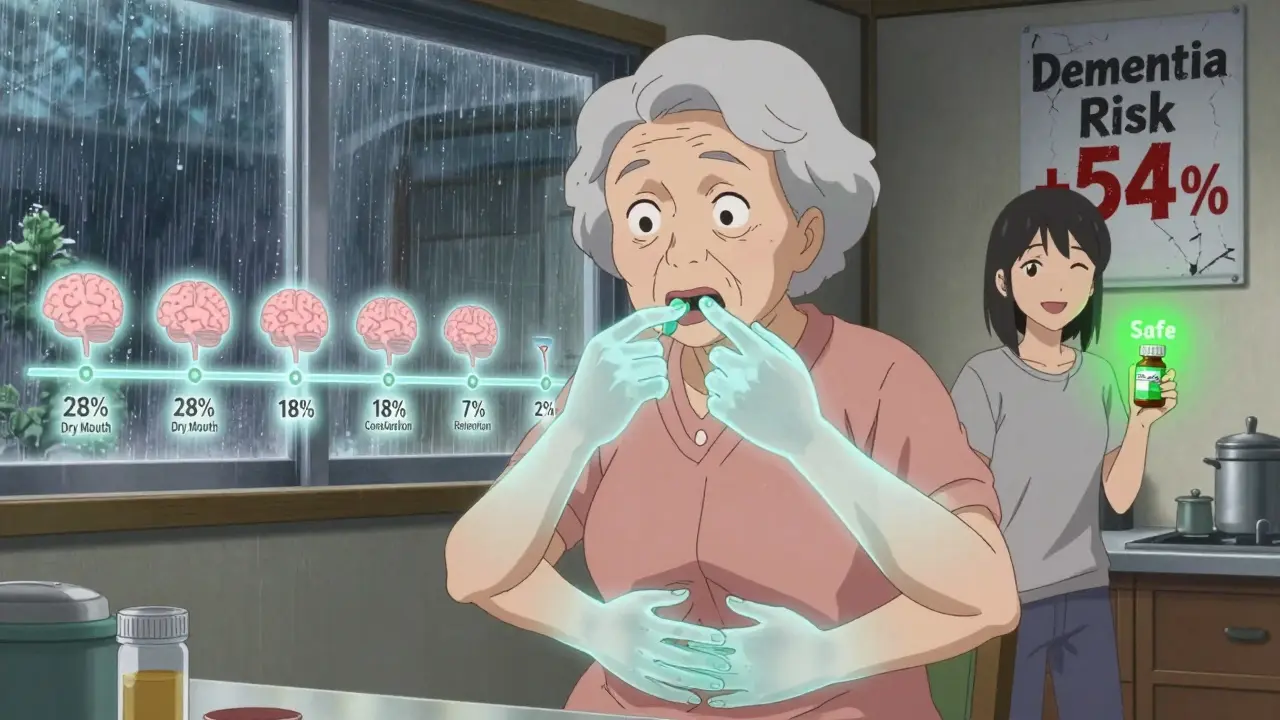
Dry mouth isn’t just about needing a sip of water. It’s a sign your body isn’t producing enough saliva. Studies show first-generation antihistamines can cut saliva flow by 60-70%. That’s not just inconvenient. It increases your risk of cavities, gum disease, and oral infections. You might not notice it right away, but over time, your teeth start to suffer. One 2019 study measured this directly: people taking diphenhydramine reported dry mouth in 28% of cases. Compare that to cetirizine (Zyrtec) at 4% and fexofenadine (Allegra) at 2%. That’s a seven-fold difference. And it’s not just about comfort. Saliva helps wash away food, neutralize acid, and protect your teeth. Without it, your mouth becomes a breeding ground for bacteria. Many people assume dry mouth is just dehydration. But if you’re drinking plenty of water and still feeling parched, the culprit might be your allergy med. The American Dental Association recommends sugar-free gum with xylitol to help. Chewing it for five minutes can boost saliva flow by 40-60%. But if you’re taking these meds daily, gum won’t fix the root problem.Constipation: When Your Gut Slows Down
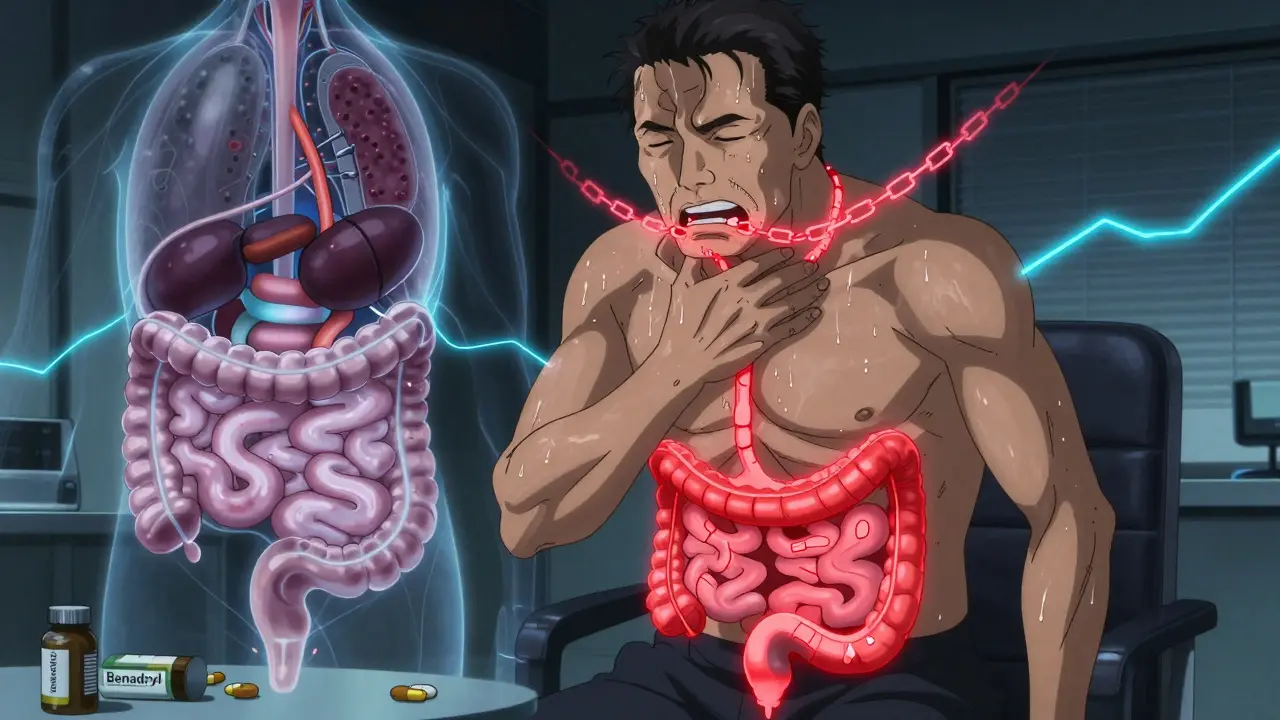
Your digestive system relies on acetylcholine to move food along. When antihistamines block it, your intestines slow down. Peristalsis-the wave-like muscle contractions that push food through-drops by 30-40%. Transit time doubles. That means you’re not just going less often. You’re struggling to go at all. Clinical data shows 15-20% of people using first-generation antihistamines develop constipation. For older adults, that number climbs higher. A 2020 study found that among patients over 65, constipation occurred in nearly one in five users of diphenhydramine. Meanwhile, second-generation options like loratadine (Claritin) caused constipation in only 3-5%. This isn’t just about inconvenience. Chronic constipation can lead to hemorrhoids, bowel obstruction, and even fecal impaction. The American Gastroenterological Association recommends taking polyethylene glycol (17g daily) as a preventive measure if you must use first-generation antihistamines. But again, that’s a band-aid. The real solution is switching to a drug that doesn’t cause this in the first place.
Urinary Retention: A Silent Crisis
This one is often overlooked-until it’s not. Acetylcholine tells your bladder to contract so you can urinate. Anticholinergic drugs block that signal. The result? Your bladder fills up, but it doesn’t know how to empty. In men with enlarged prostates, this can lead to acute urinary retention-where you literally can’t pee at all. That’s a medical emergency. Studies show 5-8% of elderly patients on first-generation antihistamines experience urinary retention. For men with an International Prostate Symptom Score above 8, that risk jumps to 31% within 48 hours. The American Urological Association says outright: avoid these drugs in men with moderate to severe prostate issues. But it’s not just men. Women can have trouble too-feeling like they can’t fully empty their bladder, needing to go more often but only passing a little, or even having urinary tract infections from retained urine. A Reddit thread from 2023 had over 37 men reporting sudden urinary hesitancy after taking Benadryl. One wrote: "I thought I had a UTI. Turns out it was the allergy pill I’d been taking for years."Generations Matter: First vs. Second
Not all antihistamines are created equal. The difference between first- and second-generation drugs isn’t just marketing-it’s chemistry. First-generation antihistamines (diphenhydramine, chlorpheniramine, hydroxyzine) were made to cross into the brain. They’re cheap, effective at causing drowsiness, and widely available. But they bind tightly to muscarinic receptors. Diphenhydramine has a Ki value of 87 nM at the M1 receptor-meaning it blocks acetylcholine almost as well as it blocks histamine. Second-generation antihistamines (cetirizine, loratadine, fexofenadine, desloratadine) were designed to stay out of the brain and avoid muscarinic receptors. Their Ki values for M1 receptors are over 1,000 nM-so weak, they barely register. That’s why dry mouth rates are 5-10 times lower. Constipation? Nearly gone. Urinary issues? Almost never reported. The numbers don’t lie:- Dry mouth: 28% (diphenhydramine) vs. 4% (cetirizine)
- Constipation: 18% vs. 4%
- Urinary retention in elderly: 7% vs. 0.8%
Why This Matters More Than You Think
These aren’t just side effects. They’re warning signs. In 2015, Dr. Shelley Gray’s team at the University of Washington found that long-term use of first-generation antihistamines like diphenhydramine was linked to a 54% higher risk of dementia over seven years. The more you took, the higher the risk. Each extra year of use above 90 daily doses added 20% more risk. The American Geriatrics Society lists diphenhydramine as a "potentially inappropriate medication" for older adults. The European Academy of Allergy and Clinical Immunology says to avoid them entirely after age 65. Mayo Clinic removed diphenhydramine from its inpatient formulary in 2022 because it was causing too many cases of delirium. Even short-term use can be dangerous. A 2023 study from the American Academy of Neurology found that taking first-generation antihistamines for more than seven days straight increased fall risk by 34% in people over 65. That’s not just about drowsiness. It’s the combo of dry mouth (leading to dehydration), constipation (causing abdominal pressure), and urinary retention (triggering bladder fullness)-all of which throw off balance and awareness.What You Should Do
If you’re taking diphenhydramine, chlorpheniramine, or promethazine regularly, ask yourself:- Do you sip water constantly?
- Do you struggle to go to the bathroom?
- Do you feel like you can’t fully empty your bladder?
Final Thoughts
You don’t need to suffer dry mouth, constipation, or urinary issues to manage your allergies. The science is clear: first-generation antihistamines are outdated. Their risks outweigh their benefits for most people. Second-generation options work just as well-without the hidden damage. It’s not about being "too sensitive." It’s about understanding what’s really happening in your body. These aren’t "normal" side effects. They’re signs that a drug is interfering with your nervous system in ways that can have long-term consequences. Your body doesn’t need to be dry, backed up, or stuck. There’s a better way.Can antihistamines cause long-term damage?
Yes, especially with long-term use of first-generation antihistamines like diphenhydramine. Research shows a 54% increased risk of dementia over seven years in adults over 65 who use these drugs regularly. The risk rises with cumulative dose-each additional year of use above 90 daily doses increases dementia risk by 20%. These drugs also contribute to chronic constipation, urinary retention, and oral health decline, which can lead to serious complications if left unaddressed.
Are all antihistamines equally likely to cause dry mouth?
No. First-generation antihistamines like diphenhydramine cause dry mouth in about 28% of users. Second-generation options like cetirizine (Zyrtec) cause it in only 4%, and fexofenadine (Allegra) in just 2%. The difference comes down to how strongly the drug binds to muscarinic receptors. Second-generation drugs were specifically designed to avoid this interaction.
Why do older adults have worse side effects?
Older adults metabolize drugs more slowly, so antihistamines stay in their system longer. Their bodies also produce less acetylcholine naturally, so blocking what’s left has a bigger impact. Plus, many seniors have pre-existing conditions like enlarged prostates, slow digestion, or dry mouth from other medications, which makes anticholinergic effects more severe and dangerous.
Is it safe to take first-generation antihistamines occasionally?
Occasional use (once or twice a year) is generally low-risk for healthy adults. But even short-term use can cause noticeable side effects like dry mouth, constipation, or urinary hesitancy. For people over 65, those with prostate issues, or those on other anticholinergic drugs (like some antidepressants or bladder meds), even one dose can be problematic. Safer alternatives exist, so there’s rarely a need to take the risk.
What should I do if I experience urinary retention?
If you can’t urinate at all after taking an antihistamine, seek medical help immediately. Acute urinary retention is a medical emergency. Stop the medication and contact your doctor or go to the ER. Do not wait. In men with prostate enlargement, this can happen within 48 hours of taking a first-generation antihistamine. Your doctor may prescribe a catheter temporarily and strongly recommend switching to a non-anticholinergic alternative.
Can I switch from Benadryl to Zyrtec without issues?
Yes, most people can switch safely. Zyrtec (cetirizine) is equally effective for allergies but causes far fewer side effects. You may feel slightly more alert, as Zyrtec doesn’t cross into the brain as easily. Some people report mild drowsiness with Zyrtec, but it’s much less common than with Benadryl. Start with the standard 10 mg daily dose. No tapering is needed-just swap one for the other.






Ive been takin diphenhydramine for years for allergies and sleep... never thought it was doin this much damage. Dry mouth? Yeah. Constipation? Constantly. Urinary issues? Oh yeah. My dentist said my teeth are rotting from the inside. I just thought I was dehydrated. This post changed my life. Switched to Zyrtec last week. No more midnight bathroom trips. My gums are already feelin better. 🙌
This is why I stopped using Benadryl cold turkey after my mom had a delirium episode from it. She was 72. Thought it was just aging. Turns out it was the allergy pill she’d been taking since 2010. We pulled it and her mental clarity improved in 72 hours. If you’re over 60 and on these meds-stop. Just stop. There are better options. Don’t wait for a crisis.
I’m a nurse. Saw this exact thing in the ER last month. Guy, 78, couldn’t pee. Thought he had a UTI. Turned out he’d been taking Benadryl every night for 15 years. Catheterized him. Told him to switch. He cried. Said he didn’t know it was the meds. This isn’t anecdotal. It’s epidemic.
In India, these meds are sold like candy. No prescription. Grandmas give diphenhydramine to kids for colds. I’ve seen kids with urinary retention from it. We need awareness. Not just in US. Global problem.
The M1 receptor Ki value thing? Yeah. That’s the real kicker. Diphenhydramine’s Ki is 87 nM. Cetirizine’s is 1,400. That’s not a difference. That’s a chasm. Pharma knew. They just marketed the sedation as a feature. It’s not. It’s a liability. And we paid for it with our kidneys, bladders, and brains.
So let me get this straight-you’re telling me the entire pharmaceutical industry is lying to us? That the FDA is asleep? That every pharmacist who recommends Benadryl is complicit? You know what? I’ve been on these for 30 years. I’m fine. Maybe your body’s weak. Or maybe you just wanna sell second-gen pills at 3x the price. I’m skeptical.
I took diphenhydramine for sleep because it was cheap. Now I can’t even swallow my own saliva in the morning. My wife said I sound like Darth Vader. We switched to Allegra. No more midnight bathroom trips. No more dry throat. No more anxiety about constipation. I didn’t know it was the pill. I thought I was just getting old.
My grandma used to say "a little Benadryl helps you sleep." I didn’t realize she was slowly poisoning herself. She had dementia. We found out she’d been taking 2 pills a night for 12 years. The research is real. I’m sharing this with my whole family.
I’m a pharmacist. I’ve seen this daily. People come in with constipation, dry mouth, urinary retention. We ask about meds. 80% say "Benadryl." We tell them to switch. They say "it’s cheaper." I get it. But $12/month for Zyrtec vs. $500/month in dental bills? Urinary catheters? Dementia? The math isn’t even close. Please, stop normalizing this.
I’m 58. Took Benadryl for allergies for 20 years. Started having trouble peeing last year. Thought it was prostate. Went to urologist. He asked if I was on anticholinergics. I said yes. He said "stop it immediately." I did. 48 hours later, I could urinate normally. No surgery. No meds. Just stopped the pill. I’m not joking. It was that fast.
My mom is 80. She’s on 3 other anticholinergics already-antidepressant, bladder med, sleep aid. Then she added Benadryl for allergies. She started wandering, forgetting names, peeing in corners. We thought it was dementia. Turns out it was drug cocktail. We pulled ALL of them. Her brain came back. Not 100%. But enough to recognize her grandchildren again. This isn’t science. It’s survival.
I didn’t know this was a thing. I thought dry mouth was just aging. My husband is 67. He’s been on diphenhydramine for 15 years. We just switched him to loratadine. He says he’s sleeping better, not worse. And his constipation? Gone. I feel like we just gave him his life back.
I’m a 70-year-old retiree. I used to take 2 Benadryl a night. Last month, I couldn’t pee. ER. Catheter. Doctor said "you’re lucky you didn’t have kidney failure." I didn’t know. I thought it was normal. I’ve been on Zyrtec for 3 weeks. I feel like a new man. No more dry mouth. No more constipation. No more panic when I need to go. If you’re on this stuff-switch. Today.
In India, we have no choice. Second-gen antihistamines are too expensive. We use diphenhydramine because it works. And it’s cheap. You can’t just tell people to stop. You have to give them access. This isn’t about science. It’s about inequality. I’m not denying the risks. But your solution ignores reality.
You people are ridiculous. This is all correlation. Not causation. Maybe people who take Benadryl are just older and sicker. Maybe dementia causes them to take more meds. You’re blaming the drug, not the lifestyle. I’ve been on it for 40 years. I’m 82. Still hiking. Still sharp. You’re just scared of cheap medicine.