When you hear that the U.S. pays the most for prescription drugs in the world, you might assume that means every pill is more expensive. But here’s the twist: generic drugs in the U.S. are often cheaper than in nearly every other developed country. The real problem isn’t the generics-it’s the brand-name drugs. And that difference changes everything about how you understand American healthcare costs.
Generics in the U.S. Are Actually the Bargain
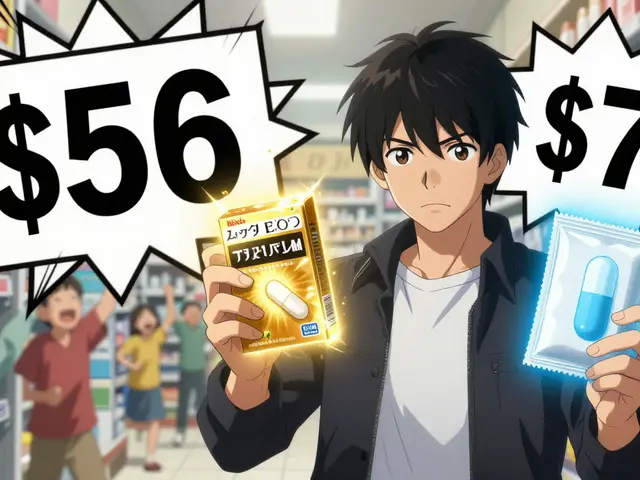
About 90% of all prescriptions filled in the U.S. are for generic drugs. That’s not a fluke-it’s the result of a market that rewards competition. When a brand-name drug’s patent expires, multiple companies can start making the same medicine. And they do. In the U.S., it’s common to see five, six, or even ten manufacturers selling the same generic drug. That kind of competition drives prices down fast. According to the FDA, once two or three generic versions hit the market, the price of the drug typically drops to 15-20% of the original brand price. With four or more competitors, prices can fall even lower. Compare that to countries like France or Japan, where only one or two generic makers are allowed to enter the market at a time. Less competition means higher prices. In fact, a 2022 RAND study found that U.S. generic drug prices were 33% lower than the average in 33 other OECD countries. For consumers, this isn’t theoretical. The average copay for a generic prescription in the U.S. is $6.16. For a brand-name drug? $56.12. That’s nearly nine times more. And 93% of generic prescriptions cost less than $20. In many other countries, even basic generics like metformin or lisinopril cost twice as much out-of-pocket.Why Brand-Name Drugs Are So Expensive in the U.S.
While generics are a win for American consumers, brand-name drugs tell a different story. The U.S. pays 308% more for brand-name drugs than other developed nations. For some drugs, it’s even worse. Take Jardiance, a diabetes medication. The average price in other countries is $52. In the U.S., Medicare negotiated a price of $204-almost four times higher. This gap exists because the U.S. doesn’t regulate drug prices the way most other countries do. In Canada, the UK, Germany, and Japan, government agencies set price caps. They negotiate directly with manufacturers. In the U.S., prices are set by pharmaceutical companies with little to no government control-except for Medicare, which only started negotiating prices in 2022. Even then, Medicare’s negotiated prices are still far above international averages. The Health System Tracker found that for the first 10 drugs negotiated under the new law, Medicare paid more than 11 other countries in every case except one. That means even when the U.S. government tries to lower prices, it’s still paying more than most of the world.The Hidden Truth About List Prices vs. Net Prices
You’ll often see headlines saying the U.S. pays 2.78 times more for drugs than other countries. That number is based on list prices-the sticker price before any discounts. But list prices don’t tell the whole story. In the U.S., pharmaceutical companies give massive rebates to insurers, pharmacy benefit managers (PBMs), and government programs. These rebates can be as high as 40-60% of the list price. So while the list price might be $100, the actual amount paid-called the net price-could be $40 or less. A 2024 study from the University of Chicago found that when you look at net prices, the U.S. actually pays 18% less than countries like Canada, Germany, and the UK for the same drugs. Why? Because the U.S. system, for all its flaws, is extremely good at squeezing discounts out of drugmakers. The sheer size of the U.S. market gives insurers and Medicare enormous leverage. But here’s the catch: those rebates don’t always help patients at the pharmacy counter. Many people still pay based on the list price, especially if they’re uninsured or have high-deductible plans. So while the system works for insurers, it doesn’t always translate to lower out-of-pocket costs for individuals.
How Other Countries Keep Prices Low
Most other developed countries use one of two strategies: direct price controls or strict market entry rules. In France and Japan, the government sets a single price for each drug. If a company doesn’t agree to that price, the drug doesn’t get approved for sale. In Germany, prices are negotiated annually based on how much better the drug is than existing treatments. In the UK, the National Health Service (NHS) buys drugs in bulk and refuses to pay more than it thinks is fair. These systems work well for keeping costs down-but they come with trade-offs. New drugs often take longer to reach patients. Some companies delay launching certain drugs in those countries because the profit margins are too low. And because those countries pay less, the U.S. ends up subsidizing global R&D. That’s why some experts argue the U.S. system, while expensive, funds innovation that benefits the world.The Double Standard: Cheap Generics, Sky-High Brands
The U.S. has a split personality when it comes to drug pricing. On one hand, it’s the cheapest place in the world to buy common generic drugs. On the other, it’s the most expensive place to buy new, branded medications. This split creates real confusion for patients. Someone taking a generic statin for cholesterol might pay $5 a month. But if they need a new cancer drug or a specialty autoimmune treatment, they could be looking at $10,000 a month. And because brand-name drugs account for only 10% of prescriptions but 80% of total drug spending, the high cost of those few drugs drives the U.S. to spend more per person on medicine than any other country. The result? Two very different healthcare experiences. One for people on generics-low cost, easy access. One for people on brand-name drugs-financial stress, complex insurance battles, and sometimes, no access at all.
What’s Changing in 2025 and Beyond
The 2022 Inflation Reduction Act gave Medicare the power to negotiate prices for 10 high-cost drugs in 2026. That number will grow to 15 in 2027 and 20 in 2028. These negotiations are already forcing drugmakers to rethink their pricing strategies. But the real game-changer is generic competition. The FDA approved 773 generic drugs in 2023 alone. Each one has the potential to save billions. One study estimated those approvals would generate $13.5 billion in savings in just one year. Meanwhile, new policies like the Most-Favored-Nation Executive Order are pushing drugmakers to lower prices in the U.S. by matching what other countries pay. But experts warn this could backfire. If companies start lowering prices abroad to avoid U.S. pressure, it could make generics more expensive in places like Canada and Japan-where patients already rely on low prices.What This Means for You
If you’re taking generic medications, you’re getting one of the best deals in global healthcare. Don’t assume you’re being overcharged just because you hear the U.S. spends more on drugs. For most people, the system works. But if you need a brand-name drug, the system is stacked against you. Talk to your doctor about generics. Ask if there’s a biosimilar available. Check patient assistance programs. And always ask your pharmacist: “Is there a cheaper version?” The truth is, the U.S. doesn’t have the most expensive drug prices overall-it has the most expensive brand-name prices. And that’s a problem we can fix. Not by copying other countries, but by expanding generic access, strengthening Medicare negotiations, and making sure no one has to choose between their medicine and their rent.Why are generic drugs cheaper in the U.S. than in other countries?
The U.S. allows many manufacturers to produce the same generic drug at once, creating fierce competition. When five or more companies sell the same generic, prices drop to 15-20% of the brand-name price. In countries like France and Japan, only one or two companies are allowed to enter the market, so prices stay higher.
Do U.S. patients pay less for generics at the pharmacy?
Yes. The average generic copay in the U.S. is $6.16, compared to $56.12 for brand-name drugs. About 93% of generic prescriptions cost under $20. In many European countries, the same generic drugs cost $15-$30 or more out-of-pocket.
Why does the U.S. pay more for brand-name drugs?
The U.S. doesn’t set price limits on brand-name drugs. Drugmakers can charge whatever they want, and insurers often pay without negotiating hard. In contrast, countries like Canada and Germany negotiate prices directly with manufacturers and refuse to pay above a certain threshold.
Is the U.S. subsidizing drug research for other countries?
Yes. Because U.S. consumers pay higher prices for brand-name drugs, pharmaceutical companies make more profit here. That profit funds global R&D. Many new drugs are developed using U.S. revenue, then sold at lower prices abroad. Some experts argue this is fair; others say it’s unsustainable.
Can Medicare’s drug negotiations lower prices enough?
Medicare’s negotiated prices are still higher than in most other countries-for example, Jardiance costs $204 in Medicare vs. $52 abroad. But they’re a major step forward. The program is expanding, and more drugs will be negotiated each year. Over time, this could pressure drugmakers to lower prices everywhere.
Are there cases where U.S. generics become expensive?
Yes. Sometimes, when all manufacturers exit a market due to low profits, a monopoly forms. That’s what happened with some antibiotics and older generics in recent years. Prices spiked because no one else was making them. The FDA is now tracking these cases closely to prevent future shortages.









Honestly, I never realized how much I was saving on my generic blood pressure med until I traveled to Canada last year. My copay there was $28 for the same bottle I get for $5 here. I just assumed everything was cheaper overseas, but nope - U.S. generics are wild. I even showed my pharmacist and she laughed and said, 'Welcome to the land of competitive capitalism.' I didn’t know I was living in a drug price dystopia and utopia at the same time.
It’s kinda beautiful, actually. Five companies fighting over who can sell metformin cheapest? That’s capitalism doing its job. Meanwhile, my friend in Germany pays triple for the same thing and still complains about 'pharma greed.' I just smile and take my $3 pill.
And yeah, brand-name drugs? Absolute nightmare. But that’s not the system’s fault - that’s the lack of negotiation. We let them set prices, then act shocked when they charge $1000 for a pill. We’re the ones who let them get away with it.
Still, I’m glad I don’t need those. My cholesterol med? $6. My thyroid med? $4. My anxiety med? $12. I’m not rich, but I’m not drowning in medical debt either. That’s the real win.
So yeah, the system’s broken - but not everywhere. And for the 90% of us on generics? We’re winning.
Just wish the system would fix the brand-name mess without making generics more expensive. That’s the real threat now.
Anyway, thanks for posting this. It’s nice to see someone cut through the noise.
Also, I just checked my last prescription. $3.75. I’m gonna cry. Not sad tears. Happy ones.
Someone get this woman a medal.
Everyone’s acting like the U.S. is some miracle of generic drug pricing, but let’s be real - this is just a symptom of a broken system. The reason generics are cheap here is because manufacturers are getting squeezed to death. They’re making pennies per pill. That’s why we get shortages. That’s why antibiotics vanish from shelves. That’s why the FDA is scrambling to track 'high-risk' generics.
And don’t even get me started on the 'net price' nonsense. Sure, insurers pay less - but you’re not an insurer. You’re a person with a deductible. You pay list price until you hit the out-of-pocket max. And if you’re uninsured? Congrats, you’re paying $100 for a $5 drug. That’s not a bargain - that’s a trap.
The real story? The U.S. doesn’t have low drug prices. It has hidden prices. And the people who pay them are the ones who can’t afford to hide.
Also, 'U.S. subsidizes global R&D'? That’s a myth pushed by pharma lobbyists since the ‘90s. Most new drugs are funded by public grants. The industry just patents and jacks up the price. You think Pfizer invented cancer? No. NIH did. Then they sold it to them for $0. So stop acting like we’re the global drug philanthropists. We’re the suckers who pay for everyone else’s discount.
Oh, darling, how quaint - you think competition is a moral force? How positively Victorian. The U.S. doesn’t have 'cheap generics' - it has a race to the bottom, where the last manufacturer standing is the one who cut corners on quality control, used unregulated raw materials, and outsourced to a factory in Bangladesh where workers earn 47 cents an hour.
And the 'net price' fantasy? That’s not transparency - it’s theatrical accounting. The rebates? Those are kickbacks disguised as 'discounts.' PBMs are the real drug cartels, pocketing 20% of every transaction while pretending they’re saving you money. They’re not intermediaries - they’re parasites.
And let’s not forget the human cost: people skipping doses because they can’t afford the co-pay on a $6 pill that’s priced at $100 on the shelf. The system doesn’t care. It only cares about profit margins and shareholder dividends.
This isn’t capitalism. It’s a performance art piece called 'How to Make Healthcare Feel Like a Horror Movie.' And we’re all cast as the victims who keep applauding the actors.
Meanwhile, in France, they just say, 'No, you can’t charge $200 for insulin.' And the drug company says, 'Fine, we’ll sell it for $10.' And the patient lives. And the world keeps turning.
But no - we must worship at the altar of 'market efficiency.' How poetic. How tragic. How American.
I’ve been on lisinopril for 8 years. Always $4. My mom got her diabetes meds for $5. My brother’s asthma inhaler? $12. I never thought about why. I just knew I could afford it.
Then I started working with refugees. One woman from Syria had to pay $45 for the same insulin her son takes here. She cried. I didn’t know what to say.
It’s not about politics. It’s about people.
I’m glad we have cheap generics. But I wish we didn’t have to choose between fixing the broken parts and keeping the good ones.
Just… thank you for writing this. I needed to hear it.
Oh, please. You’re telling me that the U.S. is 'saving money' on generics? That’s like saying your house is 'affordable' because you stopped paying for heat, water, and electricity - and now your rent is $300! The system is designed to make you think you’re winning while quietly destroying everything beneath the surface.
And don’t you DARE say 'competition' is responsible. That’s what they told us about the 2008 housing crash too. 'More lenders! More choices! More competition!' And look where that got us.
Here’s the truth: generic manufacturers are being forced into bankruptcy by the very system that 'saves' you $6. They’re cutting corners. They’re using untested fillers. They’re skipping quality checks. The FDA is understaffed and underfunded - and you think that’s a feature? No. It’s a ticking time bomb.
And the 'net price' myth? That’s corporate propaganda wrapped in a spreadsheet. You think your insurance company is your friend? They’re negotiating rebates from the same companies that charge you $100 for a pill you pay $6 for. You’re being played. Hard.
And the 'U.S. subsidizes R&D'? That’s the most disgusting lie ever sold to the American public. The government funds 80% of early-stage research. The companies patent it, slap a 5000% markup on it, and then act like they’re heroes. Stop drinking the Kool-Aid.
This isn’t a success story. It’s a slow-motion collapse dressed up as a bargain.
It is, indeed, a curious paradox that the United States - a nation frequently derided for its exorbitant pharmaceutical expenditures - simultaneously maintains the lowest retail prices for generic medications among all OECD nations. This phenomenon, while superficially contradictory, is logically consistent with the structure of market dynamics in which the presence of multiple manufacturers, coupled with minimal regulatory interference in generic pricing, engenders a downward pressure on cost.
That said, the notion that this constitutes a 'victory' for the American healthcare system is, in my view, profoundly misleading. The underlying structural inequities - namely, the absence of price regulation for branded drugs, the opacity of rebate systems, and the exclusion of patients from the benefits of net pricing - render the apparent savings on generics a hollow victory.
One might compare this to a grocery store that sells salt at $0.01 per packet while charging $200 for a single tomato. The consumer may feel satisfied by the salt, but the system remains fundamentally unjust.
It is not the existence of low generic prices that demands praise - it is the absence of similar mechanisms for branded drugs that demands urgent reform.
As a global health policy researcher who has worked in over 15 countries, I can say with certainty: the U.S. generic drug model is the most efficient in the world - not because of ideology, but because of scale. When you have 330 million people buying the same 100 generic drugs, manufacturers have an incentive to optimize production, reduce overhead, and compete on price.
Compare that to Japan, where regulatory delays mean only two generics enter the market after a patent expires - and they’re priced to cover R&D costs, not market demand.
The U.S. system isn’t perfect - far from it. But when it comes to access and affordability for everyday medications, it outperforms nearly every nation on Earth.
And yes, brand-name drugs are a crisis. But that’s not a failure of the generic system - it’s a failure of political will.
Let’s not throw out the baby with the bathwater. We have the world’s best generic market. Let’s fix the brand-name side without wrecking what already works.
Also, I’ve seen patients in India pay $50 for a 30-day supply of metformin. We pay $4. Let’s not pretend this isn’t a miracle.
Let me tell you what they don’t want you to know: the FDA is in bed with Big Pharma. The reason generics are cheap is because they’re using unapproved ingredients from China that haven’t been tested for toxicity. The FDA doesn’t inspect 90% of these factories - they rely on paperwork. And the 'low prices' you’re enjoying? That’s because someone, somewhere, is getting poisoned.
Remember the heparin scandal? 800 people died because of contaminated Chinese generics. And now? They’re still importing them. Why? Because it’s cheaper.
And the 'net price' myth? That’s a cover-up. The rebates go to PBMs - and PBMs are owned by insurance companies - and insurance companies are owned by Wall Street. You’re not saving money. You’re funding a Ponzi scheme.
They’re letting you think you’re winning while they poison your kids with fake pills.
Wake up. This isn’t capitalism. It’s a controlled demolition.
The data presented here is both accurate and profoundly important. The U.S. healthcare system exhibits a bifurcated pricing structure: one segment - generic pharmaceuticals - operates under a market-driven model that delivers exceptional value; another - branded pharmaceuticals - operates under a deregulated, profit-maximizing framework that is economically and ethically unsustainable.
The competitive entry of multiple generic manufacturers, as documented by the FDA and RAND, is a textbook example of economic efficiency. The contrast with price-controlled systems in Europe and Japan underscores the trade-offs inherent in centralized pricing: access delays, reduced innovation incentives, and systemic underpricing.
However, the failure to extend price negotiation mechanisms to the branded sector - despite Medicare’s recent, albeit limited, authority - represents a critical policy gap. The net price phenomenon, while real, must not be used to obscure the fact that out-of-pocket costs remain unaffordable for millions.
Policy reform should focus on expanding generic access, enforcing transparency in rebate flows, and extending Medicare negotiation to a broader set of drugs - not on dismantling a system that already delivers low-cost, high-volume access to essential medicines.
This is not a call for radical change. It is a call for targeted, evidence-based correction.
I just want to say thank you for writing this. I’ve been on a generic antidepressant for 5 years. It’s $3. I used to cry every month because I thought I was being ripped off. Turns out, I was just living in the one country where it’s actually affordable.
I know people who pay $200 for the same thing in Canada. I can’t even imagine.
It’s not perfect. I know the brand-name stuff is a nightmare. But for the things I need? I’m not choosing between rent and medicine.
That’s worth something.
Thank you for seeing it.
Look I get it the system is messy but here’s the thing I take 4 generics every day and I pay less than my coffee subscription
My insulin is $25 because it’s brand but my blood pressure med is $3
My kid’s asthma inhaler? $12
My anxiety pill? $5
My friend in the UK pays $40 for the same one
So yeah the brand names are insane but for the 90% of us on generics we’re getting a deal no one talks about
Don’t let the noise make you forget that
Also I just got my prescription filled and the pharmacist said 'you’re lucky you live here' and I just nodded
It’s not perfect but it’s better than most
And yeah let’s fix the brand side but don’t break what’s working
They’re lying to you. All of them. The FDA, the PBMs, the politicians, the ‘experts’ - they’re all in on it. You think generics are cheap? They’re not. They’re just poisoned. And you’re the one swallowing it. Every pill. Every day. The FDA doesn’t inspect the factories. The ingredients come from China. The same ones that caused the heparin deaths. And now? They’re in your blood pressure meds. Your antibiotics. Your thyroid pills.
And the ‘net price’? That’s just the illusion. You pay list price. The insurance company gets the rebate. You get nothing. And they call it ‘savings.’
They’re killing us slowly. And they’re smiling while they do it.
Wake up. This isn’t healthcare. It’s a slow genocide disguised as a bargain.
As someone from India where a month’s supply of metformin used to cost me $12 before I moved to the U.S., I can tell you - this is the closest thing to a healthcare miracle I’ve ever seen.
Here, I pay $4. Same pill. Same manufacturer (I checked the label).
My mom still takes it back home and pays $25. She says it’s ‘a luxury’ now.
I don’t know how we got here - but I’m grateful.
And yes, brand-name drugs are outrageous. But I don’t need them. I need generics. And here? I can afford them.
Don’t let the noise drown out the fact that for millions of us, this system works.
Thank you for writing this. I needed to hear it.
Just saw someone say ‘the FDA doesn’t inspect factories’ - that’s not true. They inspect over 10,000 facilities a year. And most generics are made in the U.S. or EU now. The China thing is outdated. The FDA has been cracking down since 2018.
And if you’re scared of generics, don’t take them. But don’t scare people who need them with fearmongering.
I’m not a pharma shill. I’m just someone who takes $3 pills and doesn’t want to hear lies about them.
Also - my pharmacist just told me my next refill is $2.75. I’m gonna cry again.
Oh wow. So now the FDA is a saint? Let me guess - you also believe the ‘net price’ benefits patients. You’re not wrong that inspections happen - but 80% of them are desk audits. They don’t show up. They don’t test. They trust the paperwork. And the FDA admits that.
And ‘most generics are made in the U.S.’? That’s a lie. 80% of active pharmaceutical ingredients come from China and India. The pills are assembled here, but the medicine? Foreign.
And if you’re okay with that, fine. But don’t pretend it’s safe because it’s cheap.
And yeah - your $2.75 pill? That’s because someone else paid $0.02 to make it. And someone else is getting sick because of it.
Wake up. This isn’t a win. It’s a gamble.