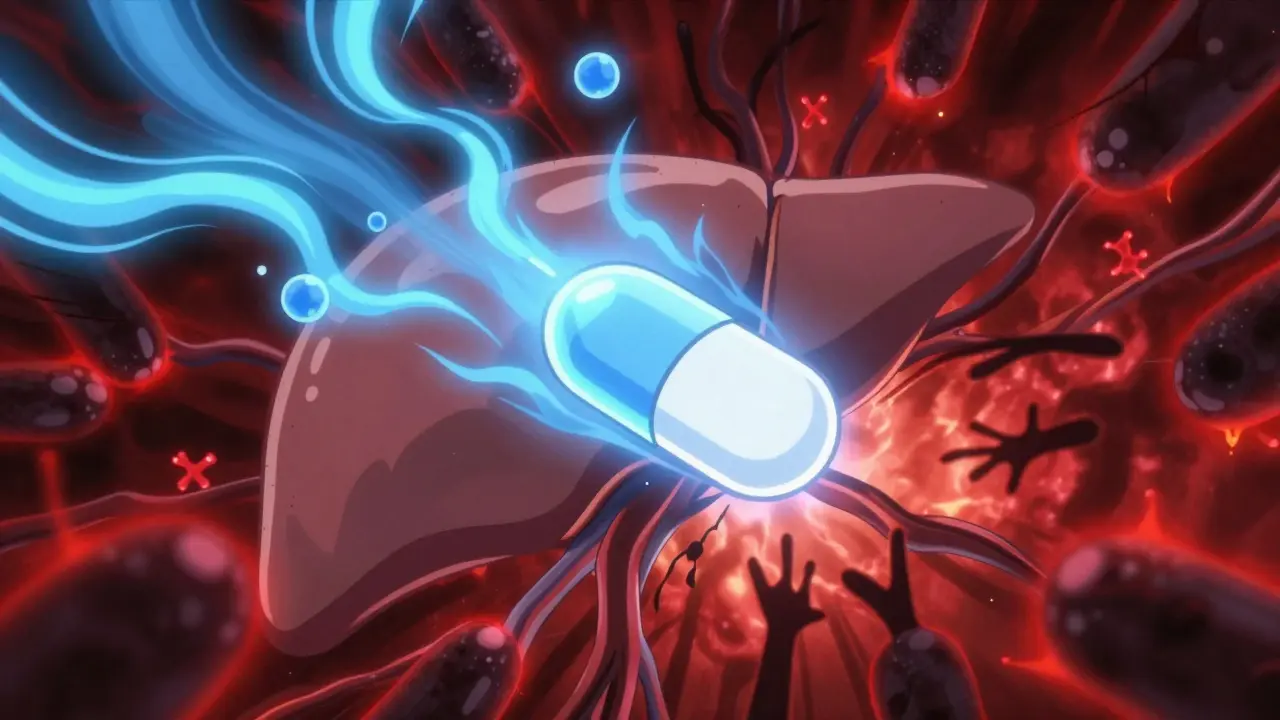
When you're taking tamoxifen for estrogen receptor-positive breast cancer, your body doesn't just use the pill as-is. It breaks it down into something far more powerful: endoxifen. This metabolite is what actually blocks estrogen in breast tissue, and it's 30 to 100 times more effective than tamoxifen itself. But here's the catch - your liver needs a specific enzyme, CYP2D6, to make endoxifen. And if you're also taking certain antidepressants, especially some SSRIs, that enzyme can get blocked. The result? Lower endoxifen levels. But does that actually mean more cancer recurrences? That’s the question doctors and patients are still sorting out.
How Tamoxifen Really Works
Tamoxifen isn't a direct cancer killer. It's a prodrug - meaning it needs to be transformed by your body to work. About 40% of its conversion into endoxifen relies on the CYP2D6 enzyme. If you're a poor metabolizer - about 7-10% of people of European descent - your body naturally makes less endoxifen. Studies show these patients have endoxifen levels 25-75% lower than normal metabolizers. But here's the twist: not everyone with low endoxifen has worse outcomes. Some large studies found no difference in recurrence or survival, even with genetically low CYP2D6 activity.
Endoxifen levels below 5.97 ng/mL have been linked to higher recurrence risk in some research, but that number isn't universal. Other enzymes like CYP3A4 and CYP2C9 can help pick up the slack, which is why some people with weak CYP2D6 still do fine on tamoxifen. The body isn't a simple on-off switch - it's adaptable. That adaptability is why the link between CYP2D6 and cancer outcomes is so messy.
Which SSRIs Block CYP2D6 the Most?
Not all antidepressants are created equal when it comes to interfering with tamoxifen. SSRIs vary wildly in how strongly they inhibit CYP2D6. The most potent offenders are paroxetine and fluoxetine. Paroxetine, in particular, can slash endoxifen levels by more than half. A 2010 Mayo Clinic study found that women taking 20 mg of tamoxifen along with 20 mg of paroxetine had endoxifen concentrations drop by 56-64%. That’s a massive hit.
Fluoxetine is also a strong inhibitor, but it sticks around in your system longer - sometimes for weeks after you stop taking it. That means even if you switch off fluoxetine, the interaction can linger. Sertraline is a moderate inhibitor, while citalopram and escitalopram are weak. Venlafaxine, though technically an SNRI, is often used as an alternative and has minimal effect on CYP2D6.
Here’s a quick breakdown:
- Strong inhibitors (avoid): Paroxetine (Paxil), Fluoxetine (Prozac)
- Moderate inhibitors (use with caution): Sertraline (Zoloft)
- Weak inhibitors (preferred): Citalopram (Celexa), Escitalopram (Lexapro), Venlafaxine (Effexor)
These aren’t just theoretical labels. They’re based on real measurements of how much each drug blocks the enzyme - measured by Ki values. Paroxetine’s Ki is 0.16 μM, making it one of the strongest CYP2D6 inhibitors known. Escitalopram’s is over 70 times higher, meaning it barely touches the enzyme.
The Conflicting Evidence: Studies That Don’t Agree
Here’s where things get complicated. Some studies say yes, this interaction matters. Others say no, it doesn’t. The 2009 Canadian study of 2,430 women found that those taking paroxetine alongside tamoxifen had a 24% higher risk of dying from breast cancer - and if they took it for more than six months, the risk jumped to 90%. That study scared a lot of doctors.
But then came the 2016 Kaiser Permanente study - a much larger one - tracking over 16,800 women for up to 14 years. It found no increased risk of breast cancer recurrence or death, even among those taking paroxetine. The Danish study of 16,254 women, published in JAMA Internal Medicine, came to the same conclusion. So did the 2023 Bayesian analysis of nearly 4,500 women: while there was a small signal of increased recurrence with CYP2D6 inhibitors, it wasn’t strong enough to confirm a real-world impact.
Why the contradiction? It comes down to how the studies were done. The smaller ones often didn’t adjust for things like cancer stage, age, or other medications. They treated SSRI use as a simple yes/no. The bigger studies looked at real-world patterns over time - tracking when people started or stopped antidepressants, how long they were on them, and whether their cancer came back later. That kind of detail changes everything.

What the Experts and Guidelines Say Now
Back in 2012, the FDA updated tamoxifen’s label to say the interaction was “theoretical” and that “available data do not establish a clinically significant interaction.” That was a quiet bombshell. Since then, the evidence has piled up in favor of that view.
ASCO’s 2022 guidelines are clear: “Clinicians should not avoid the use of antidepressants with tamoxifen due to concerns about CYP2D6 inhibition.” They say antidepressants should be chosen based on what works best for the patient’s depression, side effects, and preferences - not CYP2D6 status. The NCCN guidelines agree, but they still suggest avoiding paroxetine and fluoxetine as a precaution. Why? Because even if the risk is small, the consequences of recurrence are high.
Dr. Nancy Davidson, former president of ASCO and a leading oncologist in Seattle, put it plainly: “The totality of evidence does not support clinical concern.” Meanwhile, Dr. Richard Kim, who led the 2009 Canadian study, still advises avoiding strong inhibitors. That divide isn’t just academic - it’s shaping how patients are treated.
What Doctors Are Actually Doing
Practice is changing fast. A 2022 survey of over 1,200 U.S. oncologists showed that 68% no longer avoid all SSRIs with tamoxifen - up from just 32% in 2015. That’s a major shift in just seven years.
Paroxetine prescriptions among tamoxifen users have dropped 45% since 2010. Citalopram and sertraline have taken its place. Why? Because doctors are using the Flockhart Table - a simple chart that rates drugs by CYP2D6 inhibition strength. Many hospitals now have electronic alerts in their systems that flag paroxetine or fluoxetine when prescribed with tamoxifen. One study showed those alerts cut strong inhibitor prescriptions by 37% - without reducing antidepressant use overall.
On patient forums like Reddit’s r/breastcancer, people are still anxious. “My doctor said avoid Paxil - switched me to Lexapro and felt so much better,” wrote one user in early 2023. Others report being told to avoid all SSRIs - and feeling abandoned. The gap between fear and evidence is real. Patients need clarity, not confusion.
What Should You Do?
If you’re on tamoxifen and struggling with depression, here’s what matters most:
- Don’t stop your antidepressant without talking to your doctor. Untreated depression is dangerous - it affects your sleep, appetite, adherence to treatment, and overall survival.
- Ask about your SSRI. If you’re on paroxetine or fluoxetine, ask if switching to escitalopram, citalopram, or venlafaxine is an option. These are equally effective for depression but much less likely to interfere with tamoxifen.
- Don’t panic over CYP2D6 testing. ASCO and the FDA don’t recommend routine genetic testing. Even if you’re a poor metabolizer, you’re not automatically at higher risk.
- Focus on your mental health. Therapy, exercise, and support groups can help too. Antidepressants aren’t the only tool.
The bottom line? Your mental health matters just as much as your cancer treatment. You don’t have to choose between them. But you do need to make smart choices about which antidepressant you take.
What’s Coming Next?
The SWOG S1713 trial, expected to finish in 2025, is the first major study designed to settle this once and for all. It’s randomizing 1,500 women to either paroxetine or a placebo while taking tamoxifen - and measuring endoxifen levels directly. If endoxifen drops and recurrences go up, we’ll know for sure. If not, this whole debate may fade into medical history.
Dr. Veronique Michaud, lead author of the 2023 Bayesian study, predicts CYP2D6 testing for tamoxifen will be obsolete by 2026 - just like TPMT testing for chemotherapy drugs was abandoned after proving clinically irrelevant. The science is moving away from theory and toward real-world outcomes. And that’s good news for patients who need both cancer treatment and mental health support.
For now, the safest path is simple: treat your depression effectively, choose an SSRI with minimal CYP2D6 interference, and keep talking to your care team. You’re not alone in this - and you don’t have to sacrifice one for the other.








Tamoxifen’s entire metabolic pathway is being oversimplified by clinicians who treat CYP2D6 like a light switch. The body’s compensatory mechanisms via CYP3A4 and CYP2C9 aren’t just theoretical-they’re clinically documented in pharmacokinetic studies from 2015 onward. You can’t reduce a complex hepatic system to a single enzyme’s activity and expect real-world outcomes to follow. The Canadian study was underpowered and didn’t control for adherence, comorbidities, or tumor biology. Meanwhile, the Kaiser and Danish cohorts with 16k+ patients showed zero mortality difference. If you’re still avoiding SSRIs based on outdated pharmacology, you’re doing more harm than good.
Paroxetine’s Ki is 0.16 μM. Escitalopram’s is 11.5. That’s not a suggestion-it’s biochemistry. If you’re prescribing Paxil with tamoxifen, you’re not being cautious, you’re being negligent. The data’s been clear since 2010. Stop pretending it’s a gray area.
I’ve seen this play out in my mom’s care team-doctors scared to prescribe anything, patients left depressed and isolated. I get the concern about enzyme inhibition, but mental health isn’t a luxury. My mom switched from sertraline to escitalopram, and her mood stabilized without any recurrence signals. The real issue isn’t the drug-it’s the fear. We need to stop treating depression like a side effect to be managed and start treating it like part of the cure.
It’s funny how we treat cancer like a math problem-enzyme here, metabolite there, risk ratio there. But the body doesn’t care about Ki values. It cares about whether you’re sleeping, eating, showing up for your kid’s recital. If you’re on paroxetine and feeling like yourself again, maybe the 56% drop in endoxifen doesn’t matter as much as the 100% drop in despair. Science should serve life, not the other way around.
While the epidemiological evidence from large-scale cohort studies appears to mitigate concerns regarding CYP2D6-mediated pharmacokinetic interactions, it remains imperative to acknowledge the heterogeneity of patient populations, the potential for confounding variables in retrospective analyses, and the absence of prospective, randomized controlled trials with endoxifen as a primary endpoint. Until such data are available, clinical prudence dictates avoidance of potent inhibitors.
Oh wow, so now we’re giving cancer patients Lexapro because they’re ‘too depressed’ to care about survival? Brilliant. Let’s just swap out the chemo with a mood stabilizer and call it a day. Next up: prescribing MDMA for triple-negative breast cancer because ‘it helps with trauma.’
As a clinician who has managed over 200 patients on adjuvant tamoxifen, I can attest that the emotional burden of breast cancer is often underestimated. While pharmacokinetic interactions are scientifically valid, the psychological toll of untreated depression-manifested in non-adherence, social withdrawal, and reduced quality of life-poses a more immediate threat to long-term outcomes. The guidelines rightly prioritize patient-centered care. We must not let theoretical pharmacology overshadow lived experience.
The whole CYP2D6 thing is a distraction. Patients die from depression not from low endoxifen. Stop overcomplicating. Give them what works. Escitalopram. Venlafaxine. Done.