Over half of adults over 60 have a thyroid nodule-most don’t even know it. These small lumps in the neck are incredibly common, but hearing the word "nodule" can trigger panic. The truth? Thyroid nodules are rarely cancerous. Only about 5 to 10 out of every 100 turn out to be malignant. The real challenge isn’t finding them-it’s figuring out which ones need action and which ones can be left alone.
What Makes a Thyroid Nodule Suspicious?
Not all nodules are created equal. The key to avoiding unnecessary surgery lies in spotting the warning signs early. Ultrasound is the first and most important tool. A good scan doesn’t just show size-it reveals texture, shape, and internal details that hint at danger. Malignant nodules often have features that benign ones don’t:- Microcalcifications: Tiny white specks inside the nodule. These are found in over half of papillary thyroid cancers.
- Irregular or spiculated margins: The edges look jagged, not smooth.
- Hypoechogenicity: The nodule looks darker than the surrounding thyroid tissue.
- Vertical orientation: A nodule that’s taller than it is wide is more likely to be cancerous.
Size Matters-But Not as Much as You Think
For years, doctors were told to biopsy any nodule over 1 cm. That’s still the guideline-but it’s not the whole story. A 1.5 cm nodule with clean edges and no calcifications may be safer than a 9 mm nodule with microcalcifications. The American Thyroid Association says biopsy is recommended when:- A nodule is ≥1 cm and has suspicious ultrasound features
- A nodule is ≥1.5 cm with no suspicious features
- A nodule is ≥2 cm, regardless of how it looks
Growth Rate Is a Silent Red Flag
One of the most underused tools in thyroid nodule evaluation is time. Tracking how fast a nodule grows over months gives you more insight than a single scan. A 2017 study in the Journal of Clinical Endocrinology & Metabolism found that if a nodule grows more than 2 mm per year in two or more directions, the chance of it being cancer jumps significantly. For every extra 2 mm/year above that, the risk climbs even higher. Benign nodules grow slowly-about 1 mm per year on average. Many don’t change at all. But if your nodule grew from 10 mm to 14 mm in 12 months? That’s a red flag. Even if the first biopsy was benign, growth like this should trigger a repeat biopsy.
What Happens During a Thyroid Biopsy?
Fine-needle aspiration (FNA) is the standard. It’s quick, minimally invasive, and done right in the doctor’s office. A thin needle is guided by ultrasound into the nodule, and a few cells are sucked out. No anesthesia is needed-just a little pinch. The sample goes to a pathologist who classifies it using the Bethesda System. Here’s what the categories mean:- Category 1: Nondiagnostic (1-4% cancer risk) - Not enough cells. Repeat biopsy needed.
- Category 2: Benign (0-3% cancer risk) - Almost certainly harmless. No surgery needed.
- Category 3: Atypia of undetermined significance (5-15% cancer risk) - Unclear. Molecular testing recommended.
- Category 4: Follicular neoplasm (15-30% cancer risk) - Could be cancer. Often leads to surgery.
- Category 5: Suspicious for malignancy (60-75% cancer risk) - High chance of cancer. Surgery usually recommended.
- Category 6: Malignant (97-99% cancer risk) - Cancer confirmed. Surgery is next step.
Benign vs. Cancerous: What’s the Difference?
Most benign nodules are either:- Colloid nodules - Packed with stored thyroid hormone, often multiple and harmless.
- Follicular adenomas - Solid growths that look like normal thyroid tissue but don’t function.
- Thyroid cysts - Fluid-filled sacs. Nearly always benign.
- Papillary carcinoma - Makes up 80% of cases. Grows slowly. Often spreads to neck lymph nodes but rarely to distant organs. Highly treatable.
- Follicular carcinoma - About 10-15%. Doesn’t spread to lymph nodes but can travel to lungs or bones through the blood.
- Other types - Medullary, anaplastic, lymphoma. Rare, but more aggressive.
- A lump in your throat (globus sensation)
- Difficulty swallowing
- Shortness of breath
When Is a Biopsy Unnecessary?
Not every nodule needs a needle. Many people get nodules found by accident during an MRI or CT scan for something else. If the nodule is small (under 1 cm), looks completely normal on ultrasound, and hasn’t grown over time? No biopsy needed. Also, if you’re over 70 and have a small, stable nodule with no risk factors, your doctor might suggest watching it instead of biopsying. The risk of dying from thyroid cancer in this group is extremely low, and the risks of surgery (like lifelong hormone replacement or nerve damage) may outweigh the benefits. The goal isn’t to catch every single cancer. It’s to catch the ones that matter-the ones that could grow, spread, or cause harm. Many small papillary cancers found today would never have caused problems if left alone.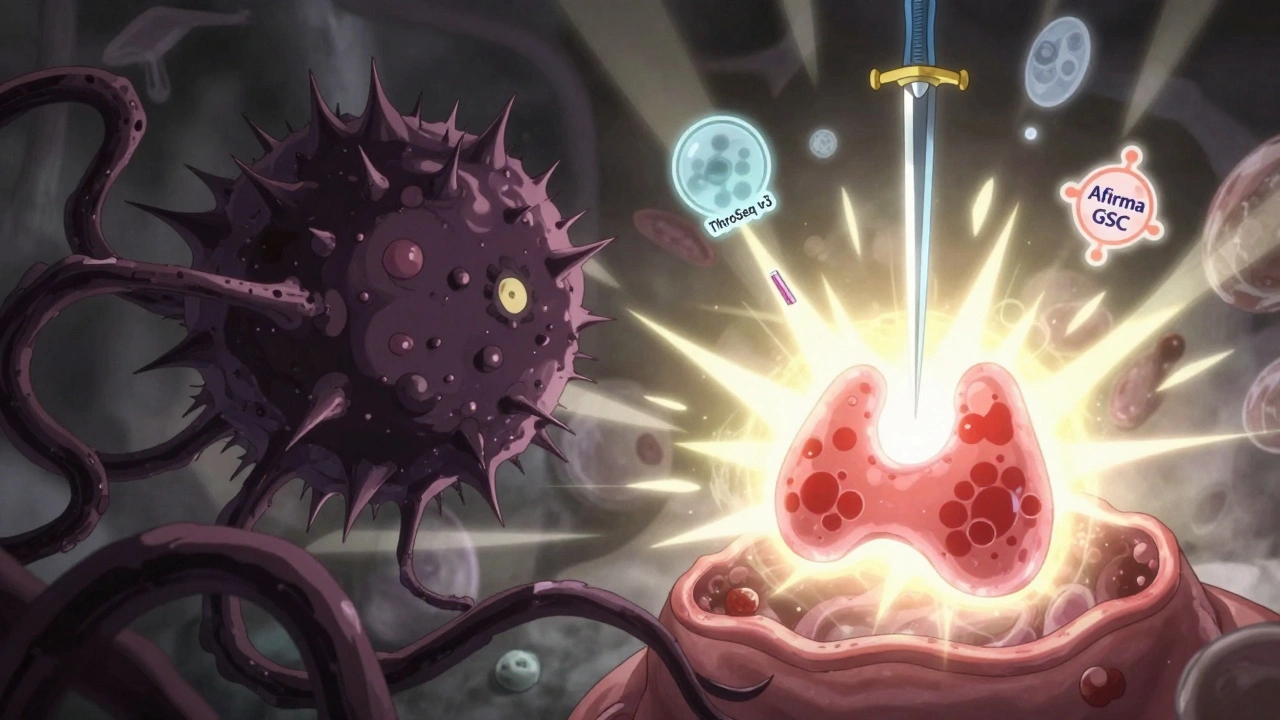
What Comes After the Biopsy?
If your biopsy says benign: You’re in the clear. Most doctors recommend a follow-up ultrasound in 6 to 12 months to make sure nothing changed. After that, yearly checks may be enough. If it’s indeterminate (Category 3 or 4): Molecular testing is your next step. If that test says low risk, you can often avoid surgery and just keep monitoring. If it says high risk, surgery is usually recommended. If it’s malignant or suspicious: You’ll likely need a thyroid lobectomy (removal of half the gland) or total thyroidectomy. Most thyroid cancers are cured with surgery and sometimes radioactive iodine. Lifelong thyroid hormone replacement is needed if the whole gland is removed.What’s New in 2025?
The field is moving fast. In 2023, the American Thyroid Association officially added growth rate as a standard criterion for biopsy decisions. Now, if your nodule grows more than 2 mm per year, your doctor should consider a biopsy-even if it was benign last time. New tools like AI-powered ultrasound analysis (like the FDA-cleared ThyroidAI platform) are helping radiologists spot subtle patterns humans might miss. These tools are about 89% accurate at predicting cancer from ultrasound images alone. And for benign nodules that cause discomfort? Radiofrequency ablation is becoming a popular alternative to surgery. It uses heat to shrink the nodule. Studies show 78% volume reduction in a year-with far fewer complications than cutting out tissue.What Should You Do If You Find Out You Have a Nodule?
Don’t panic. Don’t rush into surgery. Do this:- Get a thyroid ultrasound from a radiologist experienced in thyroid imaging.
- Ask for measurements of all three dimensions (length, width, height) and a copy of the report.
- If biopsy is recommended, ask if molecular testing is an option for indeterminate results.
- Track growth over time. Keep old ultrasounds to compare.
- Don’t accept a "just remove it" answer. Ask: "What’s the cancer risk? What happens if I wait?"








lol so now the government is putting nodules in our thyroids to control our hormones? i heard they do it through 5g towers and fluoridated water. they don't want you to know that natural iodine cures everything. just stop eating processed crap and you'll be fine. #conspiracy #freeyourthyroid
it's funny how we panic over a tiny lump but ignore the bigger stuff. maybe the real issue isn't the nodule, but how scared we are of our own bodies. i just breathe and wait. sometimes the body knows better than the machine.
the data is clear: microcalcifications + hypoechogenicity + vertical orientation = 87% sensitivity for papillary carcinoma per 2023 ATA meta-analysis. if your radiologist isn't using TI-RADS or reporting all three dimensions, they're operating at a 2010 standard. this isn't opinion-it's evidence-based triage. stop trusting 'gut feelings' and demand quantified metrics.
i had a nodule found during a car accident ct scan. no symptoms, just a quiet bump. my doctor said, 'let's watch it.' two years later, still the same size. i didn't need a needle. i needed peace. sometimes the best medicine is not doing anything.
they’re lying about the 5% cancer rate. it’s higher. they don’t want you to know the truth.
i mean... think about it. what if the thyroid is just a messenger? what if the nodule isn't the problem... it's the *message*? the universe is screaming through your neck. you're not sick-you're spiritually blocked. go to a sound bath. or cry into a crystal. the biopsy won't fix your soul.
so you're telling me i should trust a needle and a lab report more than my intuition? that's cute. i've read three books on alternative medicine and i'm pretty sure this is all just a pharma scam. also, i don't trust radiologists. they all drive bmws.
you people are pathetic. you let corporations dictate your health. if you ate real food, stopped drinking soda, and prayed to the sun like your ancestors did, you wouldn't need biopsies. this is what happens when you abandon tradition for silicon-based 'science'. shame on you.
wow. so the answer to everything is... more tests? genius. next they'll biopsy your aura. i'm just here waiting for the day they scan your dreams for cancer cells. at least my nodule is honest-it doesn't pretend to be a diagnostic tool.
you got this. whether it's benign or needs action, you're stronger than the fear. get the ultrasound. ask the questions. track your numbers. don't rush, but don't ignore. your body's telling you something-listen, but don't panic. you're not alone in this.