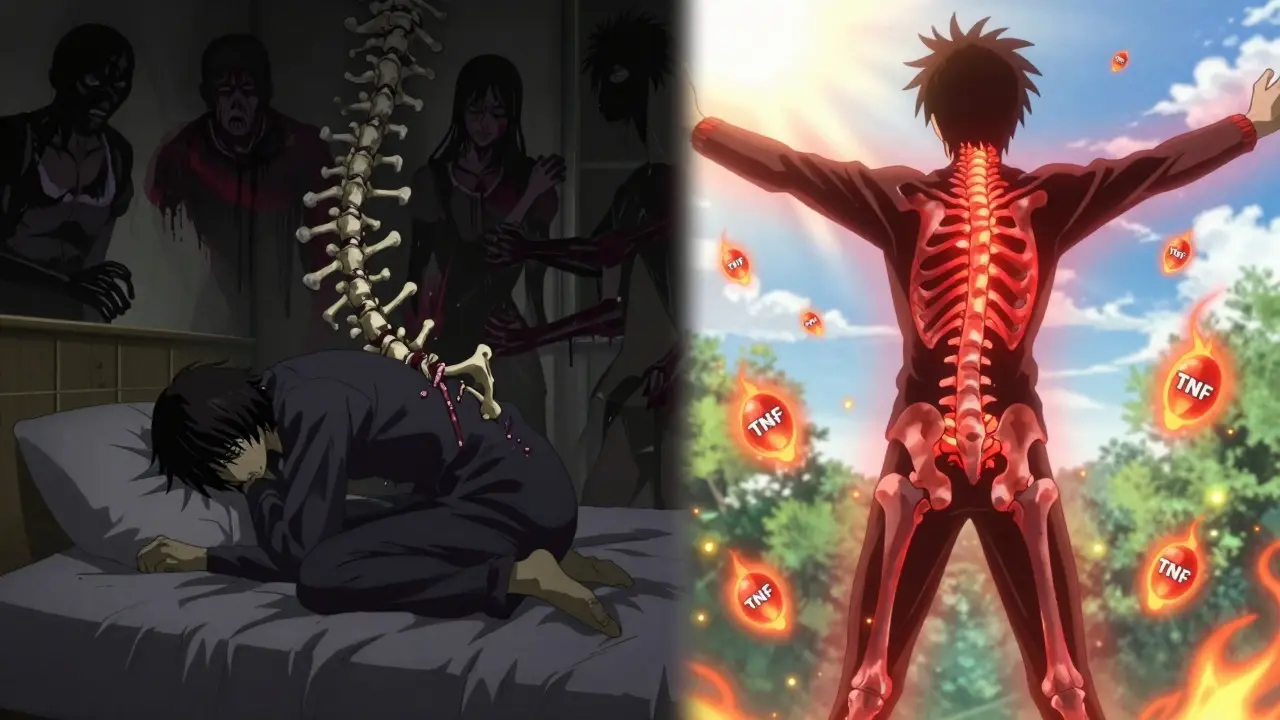
Chronic back pain that doesn’t go away with rest? Morning stiffness so bad it takes an hour to get out of bed? If you’ve been told it’s just "bad posture" or "aging," but the pain keeps getting worse - you might be dealing with ankylosing spondylitis (AS). This isn’t ordinary back pain. It’s an autoimmune disease that attacks the spine and sacroiliac joints, slowly fusing bones together and robbing people of movement. For decades, there was little doctors could do beyond painkillers and physical therapy. Then came TNF inhibitors - and everything changed.
What Exactly Is Ankylosing Spondylitis?
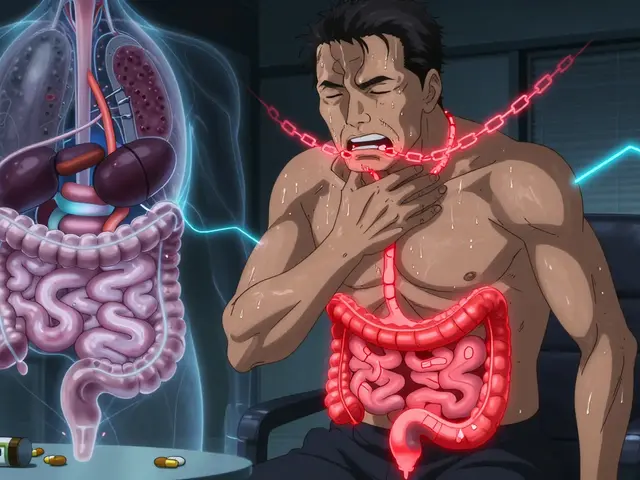
Ankylosing spondylitis is a type of inflammatory arthritis that mainly targets the spine and pelvis. Unlike osteoarthritis, which wears down cartilage, AS causes the body’s immune system to mistakenly attack its own tissues. The inflammation starts in the sacroiliac (SI) joints - where the spine meets the pelvis - and creeps up the spine over time. In severe cases, new bone forms between vertebrae, fusing them into one rigid rod. This is called syndesmophyte formation. It’s not just the spine either. AS can also affect the hips, shoulders, heels, and even the eyes.
The disease typically begins in young adulthood - between ages 17 and 45 - and is more common in men. But women get it too, often with milder symptoms that are harder to diagnose. About 90% of people with AS carry the HLA-B27 gene, though having the gene doesn’t guarantee you’ll develop the disease. Only about 5-6% of HLA-B27-positive people actually get AS. That means genetics play a role, but something else triggers the inflammation.
Early signs include:
- Chronic lower back pain that improves with movement but not rest
- Morning stiffness lasting more than 30 minutes
- Pain that wakes you up in the second half of the night
- Fatigue that doesn’t go away
- Swelling in the heels or hips
Diagnosis isn’t just about symptoms. Doctors use imaging - especially MRI - to spot inflammation in the SI joints before X-rays show bone changes. Blood tests for CRP and ESR help measure inflammation levels. The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) is a simple questionnaire doctors use to rate how active your disease is. A score of 4 or higher means your inflammation is still out of control.
Why TNF Inhibitors Are a Game-Changer
For years, treatment was limited to NSAIDs like ibuprofen or naproxen. They help reduce pain and stiffness, but they don’t stop the disease. That changed in the early 2000s when TNF inhibitors hit the market.
TNF-alpha - short for tumor necrosis factor-alpha - is a protein your immune system makes to fight infection. But in AS, it’s overproduced. It’s like a constant alarm bell in your spine, telling immune cells to attack healthy tissue. TNF inhibitors work by blocking this protein. Think of them as molecular shields that stop the inflammatory signal before it can do damage.
Five TNF inhibitors are approved for AS in the U.S.:
- Infliximab (Remicade) - given by IV infusion every 4-8 weeks
- Etanercept (Enbrel) - injected under the skin twice a week
- Adalimumab (Humira) - injected under the skin every other week
- Certolizumab pegol (Cimzia) - injected every other week or weekly
- Golimumab (Simponi) - injected once a month
Each has different pros and cons. Infliximab requires a clinic visit and takes 1-2 hours per infusion. The others can be self-injected at home. Etanercept and adalimumab have the longest track records for long-term use. Studies show that 60% of patients see a 50% improvement in symptoms within 12 weeks. MRI scans confirm inflammation in the spine drops by nearly 60% after six months of treatment.
Who Benefits Most From TNF Inhibitors?
Not everyone responds the same way. Research shows certain factors predict who will do well:
- Younger age (under 35)
- Shorter disease duration (less than 5 years)
- High CRP or ESR levels
- BASDAI score above 6
- Active inflammation on MRI
If you’ve been on maximum-dose NSAIDs for at least four weeks and still have high pain and stiffness, you’re a strong candidate. One study found that patients with both high CRP and high SAA (serum amyloid A) had an 81% chance of responding well to TNF inhibitors. That’s why doctors test these markers before starting treatment.
It’s also important to rule out infections first. All patients get screened for tuberculosis before starting any TNF inhibitor. Some people carry latent TB without symptoms, and these drugs can reactivate it. Hepatitis B and heart failure are also checked. These aren’t just paperwork - they’re life-saving steps.
Real Results: What Patients Actually Experience
Real-world data from patient forums and clinical studies tell a clear story. On the Spondylitis Association of America’s forum, 78% of over 1,200 users said their symptoms improved "substantially" after starting a TNF inhibitor. Many reported:
- Morning stiffness dropping from over an hour to under 30 minutes
- Being able to sleep through the night for the first time in years
- Returning to work, hiking, or playing with kids
One Reddit user, "BackPainWarrior," shared: "Etanercept cut my BASDAI from 8.2 to 3.1 in eight weeks. But after 18 months, I got psoriasis - had to switch to adalimumab." That’s not rare. About 15% of patients stop treatment due to side effects. Skin issues, infections, and headaches are the most common. A 2021 analysis of FDA data found infections were the leading serious side effect - especially pneumonia and skin infections.
Still, most people stick with it. A 2019 study of 429 AS patients showed the average time on TNF therapy was over 10 years. Etanercept had the highest persistence - patients stayed on it longer than any other drug. Why? Probably because it’s easy to use, has a long safety record, and works reliably.
What TNF Inhibitors Can’t Do
It’s important to be realistic. TNF inhibitors don’t cure AS. They don’t reverse fused bones. They don’t stop all bone growth forever. Studies show they reduce radiographic progression - the formation of new bone - by about half, but they don’t eliminate it. That’s why physical therapy and exercise remain essential. Stretching, swimming, and posture training help maintain flexibility even when the drug is working.
And not everyone responds. About 13% of patients are "non-responders." For them, doctors may try a second TNF inhibitor. About 30-40% of those people respond to the second one. If that fails, newer drugs targeting IL-17 (like secukinumab and ixekizumab) are now available. They work differently and can help when TNF blockers don’t.

The Cost and Access Reality
TNF inhibitors are expensive. Humira (adalimumab) used to cost over $20,000 a year. Now, biosimilars like Amjevita are available - identical drugs that cost 15-20% less. By 2022, biosimilars captured over a third of the adalimumab market in the U.S. That’s helping, but insurance hurdles remain. In Europe, 65-70% of eligible AS patients get TNF inhibitors within two years of diagnosis. In the U.S., it’s only 45-50%. Why? Prior authorization, step therapy, and high deductibles delay or block access.
Support programs exist. Specialty pharmacies offer free injection training, 24/7 nursing support, and copay assistance. The Spondylitis Association of America’s "TNF Inhibitor Starter Kit" has been downloaded over 12,000 times since 2022. It includes printable injection guides, symptom trackers, and questions to ask your rheumatologist.
What’s Next?
The future of AS treatment is moving beyond TNF blockers. New drugs targeting IL-17 are already here, and research is underway for drugs that block only the harmful form of TNF (TNFR1) while sparing the protective one (TNFR2). Phase II trials for these selective inhibitors begin in 2024. There’s also growing interest in using gene expression patterns and HLA-B27 subtypes to predict who will respond best - turning treatment from trial-and-error to precision medicine.
But for now, TNF inhibitors remain the gold standard. Over 20 years of data show they reduce pain, improve function, and lower the risk of disability. They don’t fix everything - but they give people back their lives. For many, it’s the difference between being stuck in bed and being able to walk to the mailbox, play with grandchildren, or get out of the house without dreading the pain.
Can TNF inhibitors reverse spinal fusion in ankylosing spondylitis?
No, TNF inhibitors cannot reverse existing spinal fusion. Once bone has fused between vertebrae, it’s permanent. However, these drugs can slow or reduce the formation of new bone growth (syndesmophytes) by up to 60% when started early. This is why early diagnosis and treatment are critical - before fusion occurs.
How long does it take for TNF inhibitors to start working?
Most patients notice some improvement within 2-4 weeks, especially in pain and stiffness. But full benefits usually take 3-6 months. MRI studies show inflammation in the spine and sacroiliac joints continues to decline over 6-12 months. Patience is key - this isn’t a quick fix.
Are TNF inhibitors safe for long-term use?
Yes, for most people. Over 20 years of real-world data show TNF inhibitors are generally safe for long-term use. The biggest risks are serious infections (like tuberculosis or pneumonia), skin reactions, and rare cases of heart failure or nervous system disorders. Regular monitoring - including TB screening, liver tests, and blood counts - helps manage these risks. The risk of cancer isn’t higher than in the general AS population.
What happens if I stop taking my TNF inhibitor?
Symptoms usually return within weeks. Studies show that 70-80% of patients experience a flare within 3 months of stopping treatment. This doesn’t mean you’re addicted - it means the disease is still active. If you need to stop, work with your doctor to create a plan. Never stop suddenly without medical guidance.
Can I switch between different TNF inhibitors if one doesn’t work?
Yes. If the first TNF inhibitor doesn’t help after 12-16 weeks, switching to another one is a common and effective strategy. About 30-40% of patients who fail one TNF inhibitor respond well to a second. This is why doctors don’t give up after the first try. Each drug has a slightly different structure and how it interacts with your immune system.
Do I still need NSAIDs if I’m on a TNF inhibitor?
Sometimes. Many patients continue taking low-dose NSAIDs for extra pain relief, especially during flares. TNF inhibitors control inflammation, but NSAIDs help with acute pain. Your doctor will adjust this based on your symptoms. Some people can stop NSAIDs entirely, while others need them on and off.
Is exercise still important if I’m on a TNF inhibitor?
Absolutely. Medication doesn’t replace movement. Stretching, swimming, yoga, and posture exercises help maintain flexibility and prevent further stiffness. In fact, studies show patients who exercise regularly while on TNF inhibitors have better long-term outcomes than those who don’t. Physical therapy is often part of the treatment plan.









This is why we need to stop treating AS like it's just 'bad posture.' People suffer for years before getting diagnosed. TNF inhibitors aren't magic, but they're the first real hope many of us have had.